Issue:September 2017
DRUG DEVELOPMENT - To De-Risk Patient Acceptance of Biologic Drugs, Focus Early on Delivery
INTRODUCTION
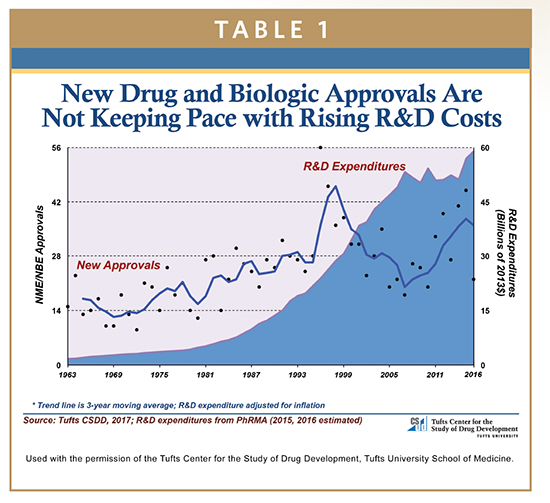
The cost of developing a new prescription drug that gains market approval has reached the stratosphere, skyrocketing 145% since 2003 – adjusted for inflation – to $2.6 billion. And the average time it takes from synthesis to approval is also a big number: 10-12 years, according to a Tufts Center for the Study of Drug Development study.1 That’s about $260 million a year to move a biologic drug candidate through the pipeline, or roughly $712,000 a day.
Most people, including government officials, know that developing new drugs is not only expensive but also quite risky. Only 7.1% of the 1,442 compounds included in the Tufts study eventually gained regulatory approval (Table 1). Despite being well aware of the extraordinary cost of biologic drug development and also of the benefits of these new treatments for patients, members of Congress continue to exert strong pricing pressure on pharmaceutical and biotech companies. Lowering drug prices became a rallying cry during the US 2016 Presidential election, and the noise hasn’t abated.
So, what does a pharmaceutical company do when everyone wants more effective new therapies but no one – including third-party payers – wants to pay the price for their development? De-risk the drug development process, in every possible way.
In the lengthy process of developing a biologic drug candidate, as with any drug, the end goal is always regulatory approval. The following discusses ways in which the path to approval is different for combination products than it is for other therapeutics and why all methods of de-risking biologics development need to occur early in the drug development process. As well, we will look at shortcuts to development time and the advantages of being first to market, not only with new drugs but also by extending a drug’s lifecycle by combining it with a device.
CURRENT DE-RISKING STRATEGIES
The pharmaceutical industry is certainly trying to de-risk drug development. Methods to make the translational stage more predictive and efficient are being employed, as are careful choices of disease projects. Extensive preclinical testing, identifying disease-state biomarkers using various analytical methods, and an integrated approach to the detection and evaluation of safety issues with comprehensive risk-analysis are standard de-risking strategies.
But biologics create even greater challenges. They are big drugs. They consist of mega-molecules that are frequently composed of a heterogeneous mixture of more than 1,300 weighty amino acids. Biologics are often hundreds of times the size of conventional small molecule drugs. Their size and complexity creates additional synthesis challenges for pharmaceutical companies seeking to develop the next blockbuster biologic.
NEW STRATEGY FOR BIOLOGIC DRUGS
These large-volume, often viscous drugs create the need for a new de-risking strategy, one that must be addressed in the early stages of the drug development process. That strategy is employing a new, patient-focused drug delivery system.
Because these large-volume drugs are not only hard to make, but also hard for patients to take, and the preferred parenteral route can be both painful and inconvenient, the pharmaceutical industry needs to address this question: how can the patient experience be improved significantly so patients are more likely to comply with prescribed therapy?
Large-volume wearable injectors provide the answer, and the pharmaceutical industry is rapidly adopting the new technology. According to a recent P&S Market Research report, the wearable injectors market is projected to reach $13 billion by 2024, growing at a CAGR of 23% until 2024.
AN ADDITIONAL DE-RISKING STRATEGY
Large-volume wearable injectors have been around for just a couple of years, and to date, only one combination product has been approved by the FDA. The most advanced of these on-body delivery devices (OBDDs) provide a compliance-boosting patient experience, yet are highly cost effective for the pharmaceutical industry, payers, and the healthcare system.
OBDD benefits and features for patients and pharmaceutical companies include the following:
-Subcutaneous self-injection of even the largest doses (10 mL to 50 mL) replacing IV infusion and significantly lowering healthcare system costs
-Enable unassisted patient self-injection of large dose biologics that is safe, easy, comfortable, and convenient
-Resolve drug development obstacles of viscosity, solubility, and protein aggregation, especially with the small-gauge needles patients prefer
-Platform for product differentiation in competitive markets
-Technology that responds to each patient by adjusting flow rate, reducing or eliminating anxiety and injection pain
-Simpler, faster product formulation for development teams
-Faster time to market
-Use of standard vials or syringes, eliminating the need for new container closure stability studies
-Multi-vial systems with practically no waste for filling the injector from standard vials or syringes
-Automatic warming of the drug as device fills – in seconds – removing the typical 30-minute waiting time for refrigerated vials to reach room temperature
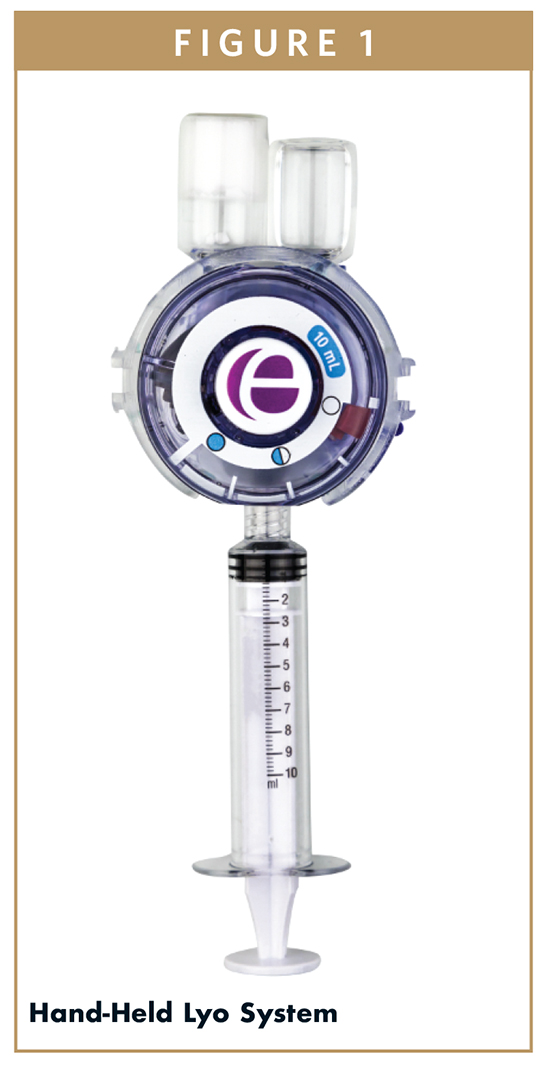
-Automatic mixing and reconstitution of lyophilized drugs, removing any patient variability from the mixing process
-Use of the smallest possible needle size possible while still delivering even the most viscous biologics with little or no discomfort
-Low profile wearables, about the size of an Oreo cookie: treatment can be administered at home, at work, or on the go with complete freedom and mobility
-Data capture to aid in monitoring patient adherence to prescribed therapy
COMBINATION PRODUCTS ADD EVEN MORE COMPLEXITY & URGENCY
Regulatory agencies are considering the new biologics delivery devices in combination with the drugs they deliver. All developers of biologic drugs, from process chemists to manufacturers, should be thinking about delivery even as the molecules are being developed and ahead of scale-up.
In fact, nearly 60% of pharmaceutical combination product experts say that the time to add the delivery device constituent is in early stages of drug development. Introducing delivery into the drug or biologic program later causes issues and compromises, according to a recent EdgeOne Medical survey.2
NAVIGATING THE REGULATORY PATH
Any experienced CRO and CMO will tell you that from day 1 of initiating a drug development project, their team is considering the most effective and efficient route to navigating regulatory paths in various countries.
In the US, as the FDA explains on the agency’s website, technological advances continue to merge product types and blur the historical lines of separation between the FDA’s medical product centers, which are made up of the Center for Biologics Evaluation and Research (CBER), the Center for Drug Evaluation and Research (CDER), and the Center for Devices and Radiological Health (CDRH).3
Because combination products involve components that would normally be regulated under different types of regulatory authorities, and frequently by different FDA Centers, they raise challenging regulatory, policy, and review management challenges. Differences in regulatory pathways for each component can impact the regulatory processes for all aspects of product development and management, including preclinical testing, clinical investigation, marketing applications, manufacturing and quality control, adverse event reporting, promotion and advertising, and post-approval modifications.
The shortest most efficient route to regulatory approval of combination devices requires that prototype delivery devices be in the lab so that device development and the evolving chemistry occur simultaneously.
DE-RISKING BY ACHIEVING FIRST-MOVER ADVANTAGE
A McKinsey & Company report examining 492 drug launches in 131 classes over a 27-year period finds a first-to-market advantage for first movers from larger pharmaceutical companies.4 They achieve a 6% market-share advantage. That advantage extends 10 years after launch, while later entrants’ advantage is in negative numbers.
Further, companies with prior experience in a therapeutic area have almost twice the first-to-market advantage as companies with no experience with that disease state. The first mover effect is strongest of all – a 13% market share advantage – when the first mover expands indications faster than later entrants in the first 5 years after launch.
Once again, OBDDs can play a significant de-risking role with their ability to reduce formulation time – by as much as a year or more, providing opportunity for the earliest possible market entry.
How? By circumventing injectable volume and viscosity limitations and by increasing the concentration of the active ingredient in the formulation. Scientists developing biotherapeutics spend enormous time and effort on formulation – sometimes years. This amount of time and effort can be significantly reduced by incorporating the newest biologics delivery technology.
The latest, most advanced large-volume wearable injector technology brings to market a novel product development aid that reduces formulation time and effort by enabling a simpler method of product preparation. Formulation teams can take advantage of the innovative delivery technology to speed development, producing stable, bioavailable, clinically relevant formulations more quickly.
At the same time, formulation teams can also facilitate patient self-injection of biologics by adopting drug delivery technology that aids in the following:
-Delivering more volume of product
-Delivering much higher viscosities caused by higher concentration of proteins
-Resolving biologics’ greater propensity to precipitate out of solution
The time and effort savings are accomplished with automated processes performed by the most advanced LVWIs, such as the Enable Injector, which accelerates or eliminates tedious, time-consuming formulation functions for more rapid – and less costly – product development.
In addition, the requirement for formulation teams to concentrate the product in the smallest possible dose for delivery by an auto-injector (typically <1 mL) may no longer be relevant. The latest generation of large-volume wearable injectors can provide a comfortable injection experience even when delivering higher volume and viscous product.
Patient acceptance of the new OBDDs should be high because the devices support mobility, are easy to use, and minimize any injection discomfort.
Prior to the introduction of large-volume wearable injectors, subcutaneous injections of biologics, the preferred route of administration, were limited in the amount and viscosity of drug product that could be delivered and tolerated by the patient in a single injection. In most cases, that volume was limited to 1 to 2 mL. Highly viscous formulations of monoclonal antibodies, for example, could not be readily injected, particularly when smaller-gauge needles are used to reduce the patient’s pain or discomfort.5,6
In contrast, these new LVWI systems overcome the large-volume injection challenges by allowing the patient to administer increased volumes into the subcutaneous space more slowly.
As well, their use of standard vials or syringes to fill the injector in a simple, intuitive way, eliminates the need for new container closure stability studies, shortening development time and speeding entry of the product to market.

DE-RISKING WITH PATENT EXTENSIONS THAT CAN ALSO WIN PATIENT LOYALTY
Already, 11 established biologic products – representing 48% of total biologic sales – are slated to lose patent protection by 2022. However, patent extension and market share protection may be possible by creating a combination product that can deliver a much higher volume of product in a single dose.
At the same time, the combination product, specifically designed to vastly improve the patient experience, can quickly create patient preference and additional marketplace advantages.
First movers who create these combination products can also differentiate not only their new and innovative commercial products, but also those products whose patents expire in the next 3 to 5 years or beyond.
WELL BALANCED PHARMACEUTICAL PORTFOLIOS NOW INCLUDE COMBINATION DEVICES
In its 2016 Pharmaceutical Industry Report, Deloitte exhorts pharmaceutical companies to embrace innovation. The consulting firm postulates that as integration of pharmaceuticals and technology continue to gain traction and accelerates, drugs will remain important but will represent a diminishing share of what comes together to deliver an overall outcome.
Disruptive innovation that can positively impact outcomes, create patient preference, and lower drug development health system costs has arrived – wearable large-volume subcutaneous injection technology. Pharmaceutical companies that embrace the OBDD technology, and their patients, have everything to gain.
SUMMARY
Pressure to reduce costs while meeting more complex regulatory mandates, as recently reported in the New England Journal of Medicine, creates the difficult challenge of developing a commercial process for a drug candidate more efficiently and within a much shorter timeframe. Some of the complexity and risk inherent in developing biologic combination products could be mitigated by incorporating a newly developed, disruptive, wearable large-volume OBDD early in the drug development process, helping not only to de-risk biologic drug uptake in patients but also bring many marketable benefits for the administration of biologics.
REFERENCES
1. Tufts. http://csdd.tufts.edu/files/uploads/Tufts_CSDD_briefing_on_RD_cost_study_-_Nov_18,_2014.pdf.
2. Edge survey.
3. https://www.fda.gov/CombinationProducts/AboutCombinationProducts/default.htm.
4. Myoung, Cha & Yu, Flora: McKinsey & Company: Pharma’s first-to-market advantage. Pharmaceuticals & Medical Products, September 2014.
5. Collins M. Here’s What’s Important About Alder Biopharmaceuticals’ Latest Release. Market Exclusive, July 26, 2016.
6. Burgess BE. Optimizing drug delivery for modern biologics. BioPharm Int. 2012;25(5). http://www.biopharminternational.com/optimizingdrug-delivery-modern-biologics.
7. Drazen JM, Harrington DP, McMurray JV, et al. The large pharmaceutical company perspective. NEJM. 2017;376:52-60.
To view this issue and all back issues online, please visit www.drug-dev.com.

Dr. Jeannie Joughin is the Vice President, Corporate Development for Enable Injections, responsible for business development, strategic alliances, alliance management, marketing, and clinical activities. She works cross-functionally to select and prioritize Enable’s global portfolio. She has also held various scientific positions, including Senior Research Scientist, Post-Doctorate and Senior Post-Doctorate positions in Australia at The Alfred Hospital, The Walter & Eliza Hall Institute, as well as internationally in Austria (University Clinic, Innsbruck) and Switzerland (Ludwig Institute for Cancer Research, Lausanne). She began her career as a Clinical Research Manager with Bristol-Myers Squibb. She moved into New Product Commercialization as the interface between the medical and marketing departments. From there, Dr. Joughin worked in Brand Management. After successfully completing several marketing roles in various organizations and companies, Dr. Joughin joined CSL Biotherapies in 2005 as Director, Pharmaceuticals Marketing and In-licensing. She assumed responsibility for a portfolio of pharmaceutical products from several licensing partners in various therapeutic areas. As Vice President, Business Development at CSL Behring, she was responsible for managing business licensing arrangements and relationships.
Total Page Views: 4354