Issue:June 2015
CLINICAL TRIALS - Accelerating the Clinical Trials Process
INTRODUCTION
The drug research and development process is a marathon. The journey from concept to FDA approval to availability typically takes upward of a decade and can cost somewhere in the neighborhood of a billion dollars. Pharmaceutical organizations are faced with time and cost complexities throughout the process, including Phase I through Phase IV clinical trials.
Reducing the time and cost of the R&D process as a whole, and of clinical trials in particular, is of paramount importance. Why is this so critical? The more companies must invest, the greater their financial exposure and risk. The longer the process takes, the greater the odds the company making the investment loses its competitive advantage. At a minimum, the window between product market introduction and patent cliff is narrowed, limiting the revenue stream before other manufacturers can enter with generics. Collectively, we should be encouraging the development of new life-altering and life-saving drugs and therapies. Instead, the clinical trials experience may discourage industry players from achieving that noble objective.
IDENTIFYING & UNDERSTANDING CLINICAL TRIALS CHALLENGES
None of this is news to pharmaceutical companies. In fact, since the turn of the century, they have executed several initiatives to cut cost and schedule. Organizations have reduced headcount, focused on process efficiency, and implemented internal collaboration portals to slash operating expenditures without sacrificing quality or compliance. They also have embraced a new business model. Rather than conducting the R&D process in-house, pharmaceutical companies are teaming with external partners to leverage their expertise and accelerate the process.
Clinical trials are a natural fit for the external partner business model, allowing companies to take advantage of the strengths of contract research organizations, laboratories, investigators, vendors, trial sites, and others. Working with these partners requires a robust collaborative operating environment. Organizations have tried extending their internal collaboration portals to address this need, with little success. The gap between internal and external collaboration is wide. As a consequence, these organizations have assumed responsibility for administrative activities and functional implementations that must be managed by IT and business owners – resulting in an increase in the very expenditures they were looking to avoid.
Organizations should take an alternate track in order to put an efficient and effective external partner collaborative environment in place. Understanding and identifying the collaborative challenges that accompany external partner-based clinical trials helps organizations recognize how to proceed to overcome those challenges.
FINDING THE RIGHT PARTNERS, INCLUDING VENDORS, SITES & PARTICIPANTS
Before a clinical trial can get off the ground, pharmaceutical companies must determine which partners and patients are qualified candidates for consideration. Viability can be a function of experience, certifications, location, financial status, compliance record, stage of illness, and other factors. Rather than conduct this background investigation before every trial, organizations need an updated registry they can access to kick-start their due diligence for partner and patient evaluation and invitation.
SELECTING & SECURING PARTNERS
The bid and proposal process, regulatory and legal requirements, and execution of master service agreements and statements of work mean the effort to bring partners into the fold can take months. In addition, convincing CROs, investigators, or sites to participate in a clinical trial is not a given because these resources possess expertise that is in demand. Successfully closing deals with partners requires making the negotiation as painless as possible. One way to do so is to make it easy for potential partners to share and sign documents throughout the negotiation. Standardized and streamlined documents, processes, and applications, along with the incorporation of new technologies like electronic data capture, also are valuable tools that minimize the administrative burden and convince prospective partners that their time can be optimized.
ON-BOARDING ORGANIZATIONS & INDIVIDUALS
Clinical trials activities necessitate the sharing of assets (applications, documents, and data) amongst pharmaceutical companies and their external partners and trial participants. Establishing “connections” that create communications paths between parties is a precursor to collaboration. How these connections are implemented directly affects the level of effort and cost required to build and maintain them. This consideration becomes particularly important as the number of partner organizations rises.
In addition, individuals must be provisioned so that they receive user accounts that allow them to access the assets of partners. Organizations have several important decisions they must make in this regard. Does each asset owner maintain its own directory of external users, or is there a central repository for all users across the clinical trial community? Are user accounts provisioned on request, or does an identity proofing event have to precede provisioning? What kind of credentials must users present in order to access assets? Is username/password sufficient, or is a stronger credential, such as a common access card or one-time password token, appropriate? The answers to these questions significantly impact on-boarding time and asset security.
CONTROLLING ACCESS
Before individuals can collaborate with their clinical trials peers by accessing assets, they must be authenticated to help verify their identities and prevent unauthorized intrusion. Asset owners need a mechanism for assigning privileges and permissions, validating credentials, and enforcing access rules, which may need to change over time as an individual’s role and responsibilities evolve on current and future clinical trials.
DEVELOPING & EXECUTING PROTOCOLS
Defining the protocols that dictate how clinical trials will be run affects decisions spanning everything from onboarding/access and patient reporting to documentation and process standards and collaboration tools/technologies. Reaching consensus mandates a high level of internal and external coordination amongst discovery teams, regulatory and health authorities, medical and clinical personnel, and others. Organizations must look for ways to shorten what has traditionally been a lengthy process. Options include dynamically created and deleted team sites for temporal information sharing and implementation of electronic or digital signatures to replace printing, ink signing, and mailing of hardcopy documents.
ACCOUNTING FOR GROWTH
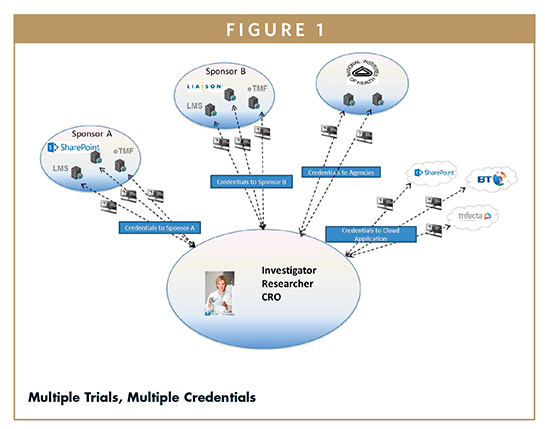
Scalability is a key consideration pharmaceutical companies must consider with respect to clinical trial time and cost. Growth is multi-faceted. The number of partners and individuals involved in a clinical trial can become quite large, making on-boarding and controlling access to assets increasingly difficult. Meanwhile, companies, their partners, and individuals all may be participating in multiple trials simultaneously. In this instance, investigators and patients may have to maintain several credentials and master different technologies, applications, and processes, as depicted in Figure 1. Collectively, these circumstances raise risk and slow efficiency. Organizations must look for ways to effectively accommodate growth without impacting performance.
BALANCING SECURITY & PRODUCTIVITY
Clinical trials require participants to share sensitive information with one another. These transactions must occur in compliance with government, industry, and corporate standards, regulations, and policies – without compromising the intellectual property that is integral to the R&D process. At the same time, collaboration cannot be so onerous that partners balk at joining the trial or individuals lose productivity. Organizations must strive for a collaborative operating environment that allows partners to connect quickly, empowers asset owners to control access, provides a simple yet compelling user experience, and accounts for the growth and dynamic needs of the community supporting clinical trials.
FACILITATING EXTERNAL PARTNER COLLABORATION WITH AN IDENTITY HUB
Clearly, building and maintaining a collaborative operating environment that addresses the challenges that accompany the conduct of clinical trials is a significant undertaking. Establishing connections, provisioning organizations and individuals, controlling access, and sharing applications, documents, and data require investments of IT resources, capital expenditures, and operating expenditures. If pharmaceutical companies and their partners attempt to create the necessary infrastructure and systems on-premises to complete these and other tasks to conduct clinical trials in a secure, seamless collaborative environment, the time and budget commitments are reminiscent of the legacy do-everything-yourself business model.
Instead, companies should look to the cloud, where they can eliminate redundancies and promote community. A hybrid cloud offers the openness and scalability of a public cloud, along with the security and control of a private cloud. A hybrid cloud-based identity hub can serve as the centerpiece for the clinical trials community of pharmaceutical companies, external partners, patients, and other participants.
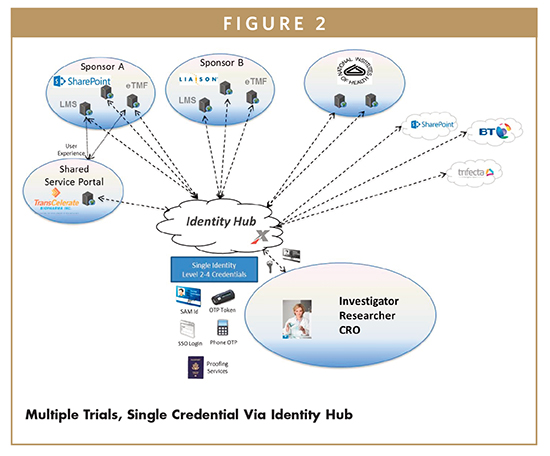
The concept of the identity hub is straightforward. Rather than spending time and money putting point-to-point connections in place with all external partners with whom they must communicate (an endeavor that scales horribly), organizations simply connect once to the identity hub, which provides the communications path to all partners. Likewise, organizations connect their relevant applications to the identity hub one time, rather than relying on multiple portals or other connection strategies.
The identity hub, in conjunction with portal service partners, also can host a registry that includes connected organizations, applications, and individuals, as well as information about vendors, sites, and patients that may not yet have participated in a clinical trial but are part of the larger scientific/R&D community. The registry contains attributes for each entity, which can span everything from certifications and geographic location to privileges and permissions for application and information access. Thus, the identity hub is perfectly positioned to work with asset owners to enforce the rules that govern access to the community’s assets by individuals involved in clinical trials.
WHO OWNS THE IDENTITY HUB?
Because the identity hub resides in the cloud rather than on-premises, pharmaceutical companies need not assume the responsibility for implementing and operating it. A viable option is to turn to an identity hub provider, who can deliver the solution as-a-Service. As a result, the identity hub provider takes the lead on establishing partner connections, provisioning organizations and individuals, and maintaining the registry or central repository that plays a key role in vendor and site selection, as well as application and information access throughout a clinical trial.
To ensure that the identity hub is aligned with regulatory and business requirements, organizations utilizing the hub service should participate in its governance. Through a delegated administration process, asset owners configure the identity hub with the privileges and permissions they wish to assign to clinical trial participants. The identity hub service encapsulates these governance rules and enforces them when individuals request access to these assets. Access requests occur when individuals present credentials to validate their identities. These credentials have been issued to individuals by an identity provider, which could be a member organization of the community, a trusted third-party connected to the identity hub, or the identity hub provider itself. The identity hub provider authenticates credentials, where the accepted types of credentials are defined by the community.
Given the nature of documentation and information shared during clinical trials, identity providers should be issuing strong credentials that align with the National Institute of Standards and Technology’s 800-63 regulations. These credentials only are provided to individuals with an existing business relationship with an inviting partner, or after the completion of an identity-proofing event, which can be conducted either in-person or remotely via webcam or an independent party like Experian. During these events, individuals confirm their identity by accurately answering personal questions and/or presenting an official government document like a passport or birth certificate. To ensure credentials meet regulatory compliance and are appropriate for use in conjunction with clinical trials, the identity provider should be certified as a Credential Service Provider by the SAFE-BioPharma Association.
Once individuals receive their credential, they can use it to conduct all clinical trials business through the identity hub, as illustrated in Figure 2. One credential significantly lessens the likelihood of loss or compromise and provides an avenue for audit of access history. It also allows for a single sign-on user experience. After the identity hub provider authenticates the presented credential, a portal service can display a dashboard for the individual that shows which applications are approved for access, which clinical trials the individual is working, and other relevant information. In fact, as use cases evolve and an individual’s role and level of security requirements change, the identity hub provider can take advantage of the dashboard to assist individuals through an automated step-up process to upgrade their one credential. By making engagement easier on individuals such as investigator site personnel, clinical trials productivity is enhanced.
The identity hub provider can deliver additional value to the community by connecting its own or trusted third-party applications to the identity hub and making them available to organizations and individuals conducting clinical trials. These applications can raise security and efficiency throughout the clinical trials process. For example, collaboration solutions offer encryption at-rest and in-transit, document version control, dynamically created team sites, and credential-controlled access to real-time audio/video conferences. The identity hub provider can leverage credentials to provide SAFE-BioPharma-compliant electronic signature functionality that empowers clinical trials participants to automate the exchange of reports, assessments, and other documents that require signatures. This capability improves security by creating a clear audit trail while simultaneously keeping trials moving by eliminating the need to print, sign, and send documents.
FROM CONCEPT TO ADOPTION
The identity hub is not a theoretical construct; it is being used today by pharmaceutical companies to help conduct clinical trials and ultimately speed new drugs to market. Merck has connected its EngageZone portal to a hybrid cloud-based identity hub hosted as-a-Service by an identity hub provider. Merck’s CRO, academic, investigator, and laboratory partners reach EngageZone by connecting to the same identity hub themselves. By embracing this approach, Merck has reduced on-boarding times for external partners from weeks or months to just days. When Merck needs to execute specific collaborative efforts with its partners, it now can create dynamic team sites in a matter of hours instead of days.
TransCelerate BioPharma, the consortium of 19 pharmaceutical companies formed to improve efficiency and productivity in clinical development, is incorporating an identity hub into its collaboration-focused solution. Access to TransCelerate’s electronic portal through which all 19 companies communicate with investigators globally will be controlled by an identity hub. The identity hub gives the pharmaceutical companies the level of security they demand to ensure their intellectual property is protected while they work with competitors to standardize industry processes and procedures that will improve clinical trials execution. Investigators will use a single credential to reach the portal and navigate a dashboard to access the applications, documents, and data associated with the clinical trials being run by each TransCelerate member with whom they work.
PUTTING IT ALL TOGETHER
Pharmaceutical companies continue to search for ways to reduce the cost and duration of the drug R&D process. That means they will stay the course on their transition to an external partner business model, playing to the strengths of CROs, laboratories, investigators, academic institutions, and others. In other words, collaboration beyond enterprise boundaries is here to stay. The demand for secure, seamless collaboration will manifest itself most acutely in the execution of clinical trials.
Making collaboration secure and seamless, while containing cost and schedule, is a challenge. Taking the wrong approach to deploying a collaborative operating environment can exacerbate the challenge, putting pharmaceutical companies and their external partners at risk. Hybrid cloud-based identity hubs, delivered as-a-Service, are proving to be an effective option for achieving all collaboration objectives. Identity hubs that serve as the foundation of the collaborative environment allow organizations to engage more quickly, while minimizing redundant infrastructure and capital expenditures. Identity hub providers ease the burden on IT and accelerate the onboarding, identity proofing/credentialing, and authentication activities that lead to greater productivity by clinical trials teams.
By improving the collaborative experience without sacrificing control or security of sensitive information or intellectual property, identity hubs and their providers help pharmaceutical companies minimize the time and cost of clinical trials and the drug R&D process as a whole. As a result, pharmaceutical companies will be better positioned to maximize new drug revenue streams, and that means more life-altering and life-saving new drugs and therapies will be available to all consumers.
To view this issue and all back issues online, please visit www.drug-dev.com.

Tom Johnson has over 25 years of experience guiding process improvement, managing technology deployment, and directing program teams in the Life Science, Healthcare, and Aerospace and Defense industries. He currently serves as Senior Director of Healthcare and Life Science Solutions at Exostar. In this role, Mr. Johnson leads the company’s Healthcare and Life Science secure business collaboration program, directing all development and implementation efforts for solutions for application and information access and protection. Exostar’s Life Sciences Identity Hub brings together over 15,000 individuals in more than 700 manufacturing, contract research organization, laboratory, and academic organizations worldwide. Mr. Johnson has a BS in Industrial Engineering from Georgia Tech University.
Total Page Views: 4973