Issue:May 2023
VACCINE TECHNOLOGY - Solving the Challenges & Introducing New Strategies for Influenza & COVID-19 Protection
INTRODUCTION
Currently available influenza vaccines have three key problems to overcome to improve their modest efficacy: their limited ability to block influenza infection and prevent the virus from spreading, short durability of immune responses, and the inability to address drifted or “mismatched” strains of flu. While vaccine developers have worked to address these problems by exploring new approaches to the design, manufacture, and/or administration of influenza vaccines, no single approach has yielded an approved vaccine that addresses all three problems.
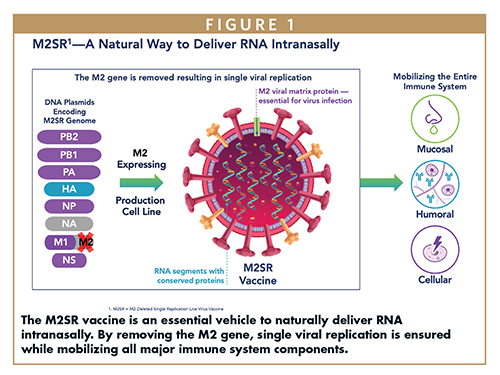
FluGen aims to change that with its M2SR (M2 Deleted Single Replication) influenza vaccine technology, which overcomes many of the limitations of today’s influenza vaccines. M2SR is based on a live but replication-deficient influenza virus delivered as an intranasal spray, resulting in broader and more durable immune responses, especially at the site of infection, and greater efficacy at preventing infection and illness.
FluGen also believes its M2SR technology can help address the shortcomings of approved COVID-19 vaccines, which are now facing some of the same challenges as influenza vaccines. FluGen is developing the M2SR technology as a vector platform for respiratory infectious diseases that includes an influenza/COVID-19 vaccine. This vaccine, either alone or in combination with other influenza and/or COVID-19 vaccines, could provide broader and more durable protection against infection by influenza and SARS-CoV-2 viruses.
The following describes where the key challenges arise for current influenza vaccines, how FluGen’s technology addresses them, and why FluGen believes combination vaccines will be key to providing ultimate protection against both influenza and COVID-19.
WHERE & WHY CURRENT INFLUENZA VACCINES FALL SHORT
Influenza vaccines fall into three broad categories: inactivated influenza vaccines (IIVs), which deliver inactivated virus by intramuscular injection; recombinant influenza vaccines (RIVs), which deliver recombinant hemagglutinin (HA) antigen, also by intramuscular injection; and live attenuated influenza vaccines (LAIVs), which contain a live but weakened virus, delivered as an intranasal spray.
The largest and perhaps most notable problem with IIVs and RIVs is their modest efficacy, which is 50%-60% at best, and well below the NIH’s target of 75%. Three factors can contribute to this limited efficacy: the vaccines’ ability to stimulate antibodies primarily against just one viral antigen, influenza A HA; the stimulation of mainly serum antibodies; and viral drift or “mismatch” between the vaccine and the circulating viruses.
The type of immune protection provided by IIVs and RIVs is a function of their manufacturing processes. For IIVs, the virus is grown in eggs, then inactivated to produce a vaccine that primarily presents HA, a surface protein the virus requires for cell entry, to the immune system. For RIVs, recombinant baculoviruses expressing HA from the viral strain of interest are grown in insect cells, and the HA is purified for use in the vaccine. Because they are delivered via injection, IIVs and RIVs elicit high titers of hemagglutinin-inhibiting (HAI) antibodies in serum. But they do not elicit serum antibodies to other important viral antigens, such as neuraminidase (NA) or nucleoprotein (NP).
Moreover, systemic HAI antibodies provide no local immunity at the site of infection, which is the nose and upper respiratory tract. This means IIVs and RIVs cannot prevent infection by the virus; they can only prevent or minimize illness arising from the infection. Intranasal LAIVs may stimulate local immunity; but because the vaccine relies on virus replication to generate protective immunity, the efficacies of these vaccines are limited in individuals who have pre-existing influenza immunity that prevents vaccine virus replication.
Viral drift is another factor that adversely affects the efficacy of all three categories of vaccines. Viral drift is the tendency for the influenza virus to accumulate changes in the HA and NA surface antigens over time. When this happens, the antibodies elicited against one strain of influenza virus eventually will not recognize and neutralize newer, “drifted” versions of the virus.
Similarly, viral drift can result in mismatches between the selection of the viral strain(s) used to manufacture the annual vaccine – which is based on predictions by the Centers for Disease Control and Prevention (CDC) and other health authorities about the strains likely to circulate during the Northern Hemisphere’s flu season – and the strains that actually circulate during flu season. When the mismatch is high, vaccine efficacy can be quite low, as was the case during the 2014-2015 flu season, when overall efficacy of the vaccine was less than 20%.
Additionally, current vaccines provide only a few months of protection, which is shorter than the actual flu season; and because they do not protect against infection – only illness – people can still contract the virus, shed it, and transmit it to others, even if they never experience any overt symptoms of infection.
M2SR: MOBILIZING THE ENTIRE IMMUNE SYSTEM WHERE IT COUNTS
FluGen’s M2SR vaccine technology addresses all of the aforementioned issues with influenza vaccines. M2SR is a live influenza virus in which M2, a protein the virus requires for replication, has been genetically deleted. The M2 protein is added back during manufacturing, allowing for production of the single replication virus. Because it is a live and intact virus, M2SR stimulates immunological responses to HA as well as NA, NP, M1, and other conserved viral antigens. But because it cannot replicate more than once in the vaccinated individual, M2SR does not lead to any viral shedding or sequelae that are associated with LAIVs based on replication-competent viruses.
While FluGen has developed all four components needed for a quadrivalent M2SR influenza vaccine, our initial clinical testing has focused on the H3N2 component, which we call H3N2 M2SR. This is because the H3N2 subtype of influenza A causes the most serious illness, especially in older adults, and current vaccines typically have the lowest efficacy against this subtype.
M2SR is delivered as an intranasal spray, which stimulates durable, local immunity at the site of infection in the form of mucosal antibodies, serum antibodies, and cellular (T cell) immunity.1,2 M2SR also elicits cross-reactive serum antibodies that were shown to last at least 6 months in clinical testing.1 M2SR to date has demonstrated an excellent safety and tolerability profile, even with a dosing window 10- to 100-fold higher than for other intranasal vaccines, because M2SR replicates only once.
Additionally, through its combination of viral antigens and intranasal delivery, M2SR elicits cross-reactive responses: that is, it remains efficacious even when the infecting strain of the virus does not exactly match the strain used to make the vaccine.
For example, last year, we published results from a Phase 2 challenge study, demonstrating that an H3N2 M2SR vaccine based on a 2007 strain protected vaccinated subjects against subsequent challenge with a highly drifted H3N2 strain from 2015.3 This ability of M2SR to circumvent the problem of viral drift is arguably its single greatest advantage over current vaccines.
We have just completed dosing and monitoring subjects in a Phase 1b trial, funded by the US Department of Defense, of H3N2 M2SR to test the hypothesis that combining our vaccine with an approved influenza vaccine will offer the best of both worlds to older adults: the local, durable immunity of M2SR; and the high titers of serum HAI antibodies elicited by injected vaccines that are essential to protecting older adult patients. To that end, the trial is evaluating the safety and immunogenicity of H3N2 M2SR alone, Fluzone High Dose inactivated influenza vaccine alone, and the combination of both vaccines, in a total of 305 adults aged 65-85. The last subject was enrolled in September, and to date, no severe adverse events have been reported.
We expect to have the immunogenicity data from the trial in the first quarter of 2023, and we hope those data will demonstrate a true breakthrough in achieving vaccine efficacy in this highly vulnerable population.
ADDRESSING THE PROBLEMS EMERGING FOR COVID-19 VACCINES
The mRNA vaccines against COVID-19 were developed with astonishing speed during the pandemic and have saved millions of lives worldwide since their approval. Their importance in combatting the pandemic is clear and cannot be overstated.
However, it is becoming equally clear that COVID-19 vaccines have many of the same weaknesses as marketed influenza vaccines. These include serum antibody immunity lasting only a few months; lack of immunity at the site of infection; lack of robust protection against drifted strains, most recently the Omicron variant of SARS-CoV-2; and lack of protection against infection, leading to viral shedding and transmission by vaccinated individuals who contract the virus.
The introduction of the bivalent COVID-19 booster, which includes the viral spike protein from the original strain of SARS-CoV-2 and its Omicron variant, is designed to provide broader protection than the original mRNA vaccines. Yet only about 13% of the US population has received the booster; and meanwhile, more than 3,000 people are hospitalized with COVID and more than 3,000 die from it every week.4 It seems we must either settle for COVID-19 becoming like influenza – endemic and not always well controlled by vaccines – or change our vaccine strategy.
One shift in strategy is already underway: recognizing the importance of local and mucosal immunity in blocking a respiratory virus, researchers have been investigating intranasal vaccines for COVID-19. A second strategy is combining influenza and COVID-19 vaccines, which would offer a single solution to both viruses, especially given that COVID-19 appears to be falling into a seasonal pattern similar to influenza.
FluGen is pursuing both strategies with an intranasal, combination vaccine for influenza and COVID-19. However, our approach differs from other combination vaccines in development, which either combine the components of individual influenza and COVID-19 vaccines or deliver mRNA from both viruses. Our approach inserts the receptor binding domain (RBD) of the SARS-CoV-2 spike protein into the DNA plasmids encoding the M2SR genome. In this way, we use M2SR as a vector to deliver a SARS-CoV-2 antigen, creating a bivalent COVID/Influenza M2SR vaccine that provides immune protection against both viruses.
In mice, we have shown an M2SR-vectored, COVID/Influenza vaccine, based on the H3N2 virus and encoding the RBD from the original SARS-CoV-2 Wuhan strain, elicited robust production of neutralizing antibodies against both Wuhan and the Delta variant, while maintaining identical titers of HAI antibodies and local immune responses to influenza as our M2SR H3N2 vaccine alone. Moreover, the M2SR-vectored vaccine not only generated mucosal IgA and IgG antibodies against Wuhan, but also against variant Omicron strains, without impeding the influenza responses. We are currently analyzing data from a study in hamsters challenged with SARS-CoV-2.
Initially, our bivalent vaccine could be used alone or as an add-on to existing influenza and/or COVID-19 vaccines, to provide the local mucosal, humoral, and cellular immunities that those vaccines do not. We are currently continuing preclinical studies of our M2SR-vectored COVID/Influenza vaccine, and plan to take the H3N2 version forward into clinical testing, as we have already gathered a great deal of clinical safety and toxicity data for the H3N2 M2SR influenza vaccine itself.
ENVISIONING A DIFFERENT FUTURE FOR INFLUENZA & COVID PROTECTION
Longer term, we envision developing a quadrivalent M2SR-vectored COVID/Influenza vaccine, in which each of the four M2SR components of the influenza vaccine could deliver an RBD from a different SARS-CoV-2 variant and/or different conserved epitopes from the viral spike protein that also elicit antibodies. Here, too, our M2SR technology has distinct advantages.
Live quadrivalent vaccines can be difficult to develop for two reasons: the potential for one viral strain in the vaccine to out-replicate the others; and the potential for one strain to be immunodominant, suppressing the immunity elicited by the other strains. Both results can compromise the ability of a live quadrivalent vaccine to provide the full range of intended immune responses.
FluGen does not expect an M2SR-vectored, quadrivalent COVID/Influenza vaccine to have these issues. Our vaccine replicates only once, so one strain cannot out-compete the others; and we have shown that each component of the vaccine generates immune responses without interfering with the responses generated by the other components. As with our influenza vaccine, a quadrivalent COVID/Influenza M2SR vaccine could be combined with other COVID-flu vaccines to generate the ultimate protection against both viruses.
With this combination vaccination strategy, the biopharma industry could truly solve the efficacy, durability, and drift problems of current influenza and COVID-19 vaccines. The strategy could also reduce or eliminate the need to predict which influenza strains will circulate during flu season, or to play “vaccine catch-up” as new SARS-CoV-2 variants of concern emerge.
Ultimately, we and FluGen envision a world in which the deadly, endemic, and pandemic influenza and SARS-CoV-2 viruses are more effectively managed, where consumers have more confidence that their vaccinations will prevent disease, and where morbidity and mortality will be greatly reduced.
REFERENCES
- Eiden J, Gordon G, Fierro C, et al. Vaccines (Basel). 2021;9(12):1388. doi: 10.3390/vaccines9121388.
- Eiden J, Fierro C, Schwartz H, et al. J Infect Dis.; published online Nov. 9, 2022. 10.1093/infdis/jiac433.
- Eiden J, Volckaert B, Rudenko O, et al. J Infect Dis. 2022;226(1):83-90. doi: 10.1093/infdis/jiab374.
- According to the CDC website: https://covid.cdc.gov/covid-data-tracker/#datatracker-home. Accessed Feb. 7, 2023.

Paul Radspinner is Co-founder, President, and Chief Executive Officer of FluGen Inc. As President & CEO, FluGen has raised over $40 million in capital and completed multiple human clinical trials with M2SR. After completing his MBA at Northwestern University’s Kellogg Graduate School of Management, he spent over 15 years in management roles overseeing international pharmaceutical operations, marketing, and business development with Eli Lilly and Company. After his time at Lilly, he managed the pharmaceuticals portfolio, including Vitamin D analogs at the Wisconsin Alumni Research Foundation (WARF) for the University of Wisconsin-Madison. He entered the Madison biotech scene when he took on the role of Vice President of Business Development for Deltanoid Pharmaceuticals, Inc. and then started FluGen. In 2008, he was elected to the Board of Directors for BioForward, the Wisconsin state biotechnology organization, where he served as President. He is a member of the Boards of Directors for Plumb Pharmaceuticals and Co-D Therapeutics.

Dr. Pamuk Bilsel is Chief Scientific Officer at FluGen Inc., bringing nearly 15 years of corporate biotechnology and management experience in vaccine research against infectious diseases. Prior to joining FluGen, she was involved in developing DNA vaccines based on cell-mediated immunity against influenza and malaria at Pharmexa-Epimmune, where she served as Director of Molecular Biology. At Pentamer Pharmaceuticals, a San Diego start-up venture, she worked on subunit vaccines against respiratory syncitial virus using virus-like particle technology. Preceding that, she worked at Aviron generating live attenuated influenza vaccine strains in addition to studies with the cold-adapted influenza vaccine which was eventually launched as MedImmune’s FluMist. She earned her PhD in Cell and Molecular Biology from the University of Nevada, Reno, and completed her post-doctoral training at St. Jude Children’s Research Hospital with Dr. Kawaoka.
Total Page Views: 2954










