Issue:October 2018
TRANSDERMAL DELIVERY – Effect of Skin Model on In Vitro Performance of an Adhesive Dermally Applied Microarray – ADAM(TM) – Coated With Zolmitriptan
INTRODUCTION
The in vitro human skin finite dose model, Franz, has demonstrated effectiveness in evaluating percutaneous absorption and assessing the pharmacokinetics of topically applied medicines. The model utilizes ex vivo human skin affixed to a bespoke diffusion cell that allows the skin to be kept at a temperature and humidity representative of in vivo conditions.1 A finite dose (eg, 2 mg/cm2-10 mg/cm2 of a semisolid or a transdermal delivery system) of a formulation is placed onto the exterior surface of the skin and drug absorption is quantified by measuring the amount in the receptor solution. The total absorption, absorption rate, and skin content can be evaluated in this model. The method has precedent for accurately estimating in vivo percutaneous absorption kinetics.2,3 The Franz cell has been utilized to evaluate microprojection facilitated drug delivery, employing ex vivo skin of varying thickness as the diffusional barrier.4,6 Artificial membranes, eg, Silescol®, have also been proposed as a potential substitute to ex vivo skin.7,8 The apparent benefits of employing artificial membranes are their availability, ease of use, and ease of storage. They may also lessen the variability concomitant with the use of ex vivo skin.9 Although artificial membranes may have some benefits over human skin, definite correlation to human stratum corneum barrier function has not been completely explored, particularly for finite dose applications.10
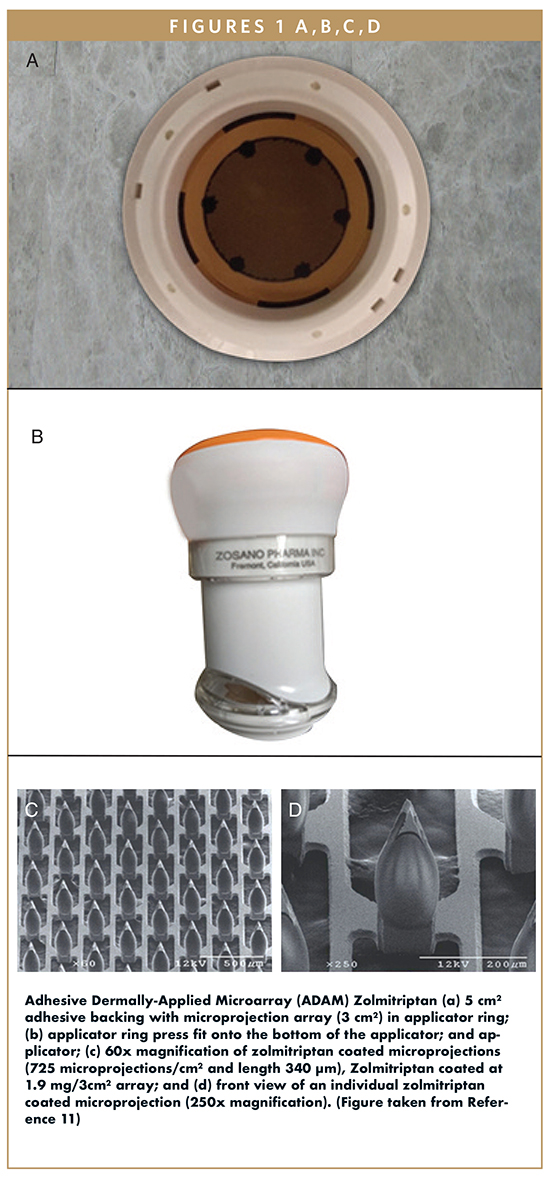
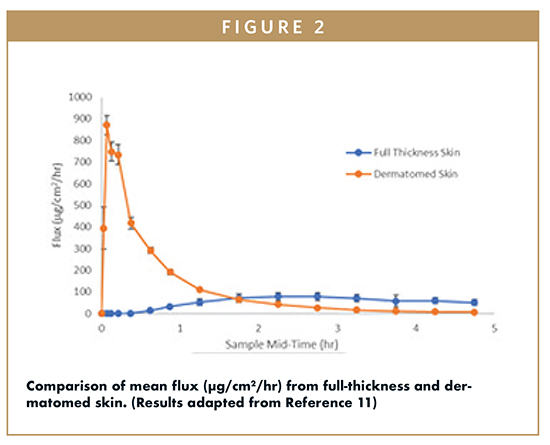
In the present study, we assessed Strat-M (artificial membrane), full-thickness, and dermatomed ex vivo skin on percutaneous delivery of zolmitriptan from innovative drug-coated dermally applied microprojections that target the epidermal/dermal layer for fast and efficient delivery.11 The Adhesive Dermally-Applied Microarray (ADAMTM) system is composed of a titanium microprojection array adhered to an adhesive backing held in a retainer ring, and an applicator (Figure 1a). The adhesive backing in the retainer ring is docked to the applicator. The applicator (Figure 1b) is actuated through a spring force, which breaks the adhesive from the retainer ring and applies the patch onto the skin site. The drug-coated microprojections physically break through the stratum corneum and penetrate into the epidermis and dermis, where the dry drug coating is dissolved by the surrounding skin interstitial fluid. The ADAM system was recently evaluated in a Phase 2 clinical study with the delivery of zolmitriptan for the treatment of migraines.12
RESULTS
Franz cell experiments are typically employed to evaluate both in vitro bioavailability and bioequivalence of topical semisolid formulations and transdermal systems. One critical use of Franz cell experiments is to optimize formulations to improve percutaneous delivery.14 Consequently, drug permeation through ex vivo skin should provide an estimate of in vivo percutaneous absorption. Nevertheless, the absence of a vascular system in an ex vivo environment signifies that the distance from the stratum corneum to its boundary with the receptor media may contain an additional unstirred barrier to drug permeation for some molecules. In an in vivo model, the distance is 200-400 μm from the stratum corneum to the dermis, where the greatest amount of drug is systemically absorbed via the capillaries.15 Therefore, a crucial characteristic of an ex vivo percutaneous absorption experiment is a judicious consideration of the membrane utilized to model in vivo skin conditions.14
To assess the influence of the skin model on microprojection mediated delivery, full-thickness skin (0.70 ± 0.09 mm thickness), dermatomed skin (0.46 ± 0.09 mm) and Strat-M® (0.30 ± 0.01 mm thickness) were used. Figure 2 compares the percutaneous absorption of zolmitriptan through full-thickness and dermatomed ex vivo human skin over a period of 5 hours.
The absorption of zolmitriptan from the two skin sources are significantly different. The time to maximum flux was much slower with the full-thickness skin in contrast to the dermatomed skin. The time to maximum flux and the shape of the curve for the full-thickness skin substrate are in stark contrast to what has been conveyed by Kellerman, et al 16 in a Phase 1 clinical study of ADAM Zolmitriptan, where the median Tmax was 20 minutes.16 The distinction between the time to peak flux is that with in vivo skin, the apices of the microprojections are near to the capillary plexus of the dermis. This allows for fast release of drug into the blood stream compared to full-thickness in vitro skin that lacks the blood flow and results in the drug having to diffuse through the full dermis to the receptor solution. Utilization of dermatomed skin, where the lower region of the dermis at the capillary bed has been removed, is a better in vitro skin model because when the drug reaches that area, it finds the receptor solution rather than the capillary blood flow, which, in either case, provides sink conditions. The results show that the use of dermatomed skin resulted in the greatest extent of intracutaneous delivery in comparison to full-thickness skin. The data indicate that the diffusion of zolmitriptan across the full-thickness skin demonstrates how the dermis, without capillary flow, will result in a rate limiting step in absorption of microprojection facilitated drug delivery attributable to the increased diffusional path length associated with the utilization of full-thickness skin.17,18
Figure 3 compares the percutaneous absorption of zolmitriptan through Strat-M® synthetic membrane versus dermatomed ex vivo human skin over 5 hours. The Strat-M membrane and the dermatomed skin permeation curve profile are analogous. However, the peak flux for the Strat-M is considerably lower than that of dermatomed skin. This singularity of low absorption across artificial membranes has been reported elsewhere and was associated with the high elasticity of the artificial membrane that causes the microprojections to retract, which means that the microprojections do not reside within the created conduits.8 Similarly, adsorption of the zolmitriptan to components of the synthetic membrane, ca 40% of the applied dose recovered in the membrane versus <1% in the epidermal and dermal layers of the dermatomed skin, may also be a contributing factor. As a result, the use of Strat-M membrane inaccurately represents the absorption in vivo and can lead to a significant under estimation of the drug release profile.
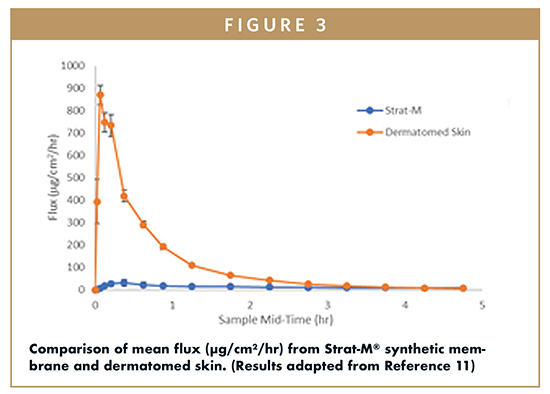
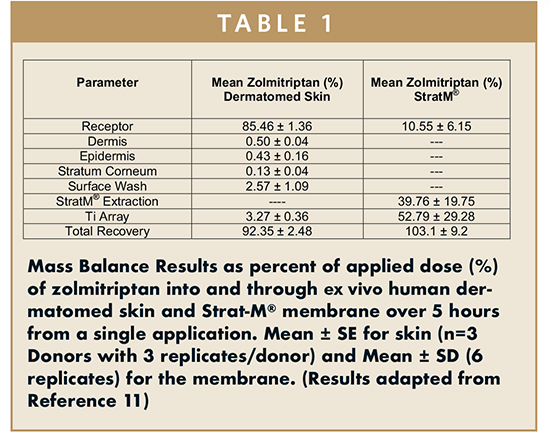
Table 1 shows the mass balance of 1.9 mg ADAM Zolmitriptan that was applied to dermatomed skin and to Strat-M membrane. For dermatomed skin, the total recovery was 92% with total absorbed zolmitriptan of 85%. Negligible amount of drug was found on the stratum corneum and on the titanium array post administration. In contrast to the skin data presented in Table 1, the amount found in the receptor media for the Strat-M condition was approximately 11% of the nominal 1.9-mg zolmitriptan dose. Most of the dose resided on the titanium array (ca 53 %), and the remainder was on the surface or within the Strat-M membrane (ca 40%).
CONCLUSIONS
This study, the first to be conducted with microneedles coated with zolmitriptan, verified the effect of in vitro experimental conditions on the rate and magnitude of permeation of ADAM zolmitriptan. The outcome of the investigation indicates that artificial membranes such as Strat-M should be utilized with caution when assessing drug release from coated microprojections that are intended to deposit their drug locally via dissolution. Dermatomed skin may be a more representative measure of in vivo performance, not only for drug-coated metallic microprojections, but also a more representative approach for most in vitro absorption studies with this delivery system. The results of this study will further inform investigators with respect to modeling the in vitro performance of other formulations and their desired delivery profile, which can be used as a tool for screening prior to advancing to studies in humans.
REFERENCES
- Franz TJ. Percutaneous absorption: On the relevance of in vitro data. J Invest Dermatol. 1975;64:190-195.
- Franz TJ. The cadaver skin absorption model and the drug development process. Pharmacopeial Forum. 2008;34(5):1349-1356.
- Franz TJ, Lehman PA, Raney PA. Use of excised human skin to assess the bioequivalence of topical products. Skin Pharmacol Physiol. 2009;22:276-286.
- Park JH, Allen MG, Prausnitz MR. Polymer Microneedles for controlled release drug delivery. Pharm. Res. 2006;23:1008-1019.
- Verbaan F, Bal S, Van den Berg D, Groenink W, Verpoorten H, Luttge R. Assembled microneedle arrays enhance the transport of compounds varying over a large range of molecular weight across human dermatomed skin. J. Control. Rel. 2007; 117:238-245.
- Donnelly RF, Garland MJ, Morrow DIJ, et al. Optical coherence tomography is a valuable tool in the study of the effects of microneedle geometry on skin penetration characteristics and in skin dissolution. J. Control. Rel. 2010;147:333-341.
- Coulman SA, Antsey A, Gateley C, et al. Microneedle mediated delivery of nanoparticles into human skin. Int. J. Pharm. 2009;366:190-200.
- Garland MJ, Migalska K, Mahmood TMT, et al. Influence of skin model on in vitro performance of drug loaded soluble microneedle arrays. Int. J. Pharm. 2012;434:80-89.
- Huong S, Bun H, Fourneron J, Reynier J, Andrieu V. Use of various models for in vitro percutaneous absorption studies of ultraviolet filters. Skin Res. Techol. 2009;15:253-261.
- Karadzovska D, Riviere JE. Assessing vehicle effects on skin absorption using artificial membrane assays. Eur. J. of Pharm. Sci. 2013;50:569-576.
- Ameri M, Lewis H, Lehman P. J. Pharmaceutics. 2018. https://doi.org/10.1155/2018/7459124.
- Spierings ELH, Brandes JL, Kudrow DB, et al. Randomized, double-blind, placebo-controlled, parallel-group, multi-center study of the safety and efficacy of ADAM zolmitriptan for the acute treatment of migraine. Cephalalgia. 2017;38(2): 215-224.
- Daddona PE, Matriano JA, Mandema J, Maa YF. Parathyroid hormone (1–34)-coated microneedle patch system: Clinical pharmacokinetics and pharmacodynamics for treatment of osteoporosis. Pharm. Res. 2011;28:159-165.
- Friend DR. In vitro skin permeation techniques. J. Control. Rel. 1992;18:238-248.
- Scheuplein RJ. Mechanism of percutaneous absorption II: transient diffusion and the relative importance of various routes of skin penetration. J. Invest. Dermatol. 1967;48:79-88.
- Kellerman DJ, Ameri M, Tepper SJ. Rapid Systemic Delivery of Zolmitriptan using an Adhesive Dermally Applied Microarray. Pain Management. 2017;7:559-567.
- Fukushima K, Ise A, Morita H, Hasegawa R, et al. Two layered dissolving microneedles for percutaneous delivery of peptide/protein drugs in rats. Pharm. Res. 2010;28:7-21.
- Banga AJ. Transdermal and intradermal delivery of therapeutic agents. CRC press, Boca Raton.
To view this issue and all back issues online, please visit www.drug-dev.com.

Hayley Lewis is the Senior Vice President of Operations at Zosano Pharma, where she oversees the functional areas of Nonclinical, R&D, Analytical Development and QC, Operations and Engineering, Manufacturing, and Regulatory Affairs, and continues to be responsible for overseeing all regulatory interactions with the FDA and other government agencies. She joined the company as the Vice President of Regulatory Affairs and Quality in October 2015. Prior to joining Zosano, she spent over 11 years in Regulatory Affairs at Depomed, Inc., a specialty pharmaceutical company, where she was involved in the approval of 3 commercial products. Over the course of her career, she has enabled 8 investigational products to be studied in humans, 5 of which have advanced to completion of Phase 3 trials. Her pharmaceutical development experience, spanning over 20 years, covers solid oral dosage forms, and combination products, such as systemic and local inhalation products, a single- entity combination injectable, and transdermal systems. Ms. Lewis earned her BS in Pharmaceutical Sciences from the University of Greenwich in England, and has attained several management diplomas from Kellogg School of Management, as well as Stanford’s Graduate School of Business.

Dr. Mahmoud Ameri is the Vice President of Research & Development at Zosano Pharma. As one of the company’s Co-founders, he brings 20 years of drug delivery, preclinical, and early ex US clinical development of combination products to the company. He is responsible for research and development. Prior to Zosano, he was at Alza/J&J were he co-invented and developed the Adhesive Dermally Applied Microarray system and holds over 20 patents and patent applications all relating to the Zosano drug delivery technology. Dr. Ameri earned his PhD from the School of Pharmacy at the University of Manchester in the United Kingdom.
Total Page Views: 4008










