Issue:March 2024
THERAPEUTIC FOCUS - TTHX1114: Improving Outcomes for High-Risk Patients After Cataract Surgery
INTRODUCTION
Cataracts are one of the most common ailments of old age.1 The condition, which is caused by the degradation of proteins in the lens of our eyes, creates a progressively opaque mass in the center of a person’s vision, blurring and obscuring vision. Without proper treatment, it can lead to major problems with sight: In 2020, an estimated 15 million cases of blindness worldwide were attributed to the disorder. The prevalence of cataracts is similar around the world, but the majority of blindness occurs in low- and middle-income countries, primarily due to limited access to quality eye care services and a shortage of trained professionals.2
Fortunately, in areas with access to modern ophthalmic care, treatment for cataracts is relatively routine. A proven and straightforward surgical procedure can remove the damaged lens and replace it with a new one, restoring sight in most individuals. In the US, more than 4 million people undergo this operation annually with remarkable success. While the surgery is generally safe and effective, there are still certain risks associated with the procedure, particularly in patients with pre-existing ocular conditions, advanced age, and systemic diseases like diabetes.3
POST-SURGICAL COMPLICATIONS IN HIGH-RISK CATARACT PATIENTS
In high-risk cases, surgery may replace one problem with another as oxidative stress from the surgical procedure damages sensitive endothelial cells that line the back surface of the cornea. Even under ideal conditions, these cells can be damaged and slowly recover, but in people with pre-existing corneal disease or advanced cataracts, the insult to the cornea’s endothelial layer from surgery is larger than usual, leading to corneal edema that can defocus light coming into the eye. This creates visual impairment that may lead to long-term follow-up treatment and prolonged compromise of daily activities.
High-risk patients face the risk of corneal endothelial damage via ferroptosis, a process that triggers cell death.4 When sensitive eye tissues are disturbed during cataract surgery, reactive oxygen species (ROS) accumulate nearby, oxidizing the lipid membranes of corneal cells and triggering the release of iron inside the cell. This phenomenon hinders the cells’ ability to neutralize oxidative molecules, while allowing excess iron to accumulate inside of them. The resulting biochemical reactions can damage or kill the cell.
If edema associated with ferroptosis occurs after cataract surgery, the consequences can include increased inflammation, delayed wound healing, and compromised visual outcomes. These side-effects can prolong recovery time and potentially affect the overall success of the surgery. Fixing the problem permanently often requires long-term follow-up treatments, or in a worst-case scenario, a corneal transplant, requiring patients take immunosuppressant drugs for the rest of their lives.
REASONS FOR DELAYED HEALING AFTER HIGH-RISK CATARACT SURGERY
Under ideal conditions, the body initiates a healing response immediately after tissue damage, releasing a molecule called Fibroblast Growth Factor 1 (FGF1). This molecule, also called acidic fibroblast growth factor (aFGF), stimulates the proliferation and migration of various cell types involved in wound healing, such as endothelial cells, keratocytes, and epithelial cells.
FGF1 can also modulate the inflammatory response in the cornea, influencing immune cells like macrophages and modulating their production of cytokines and growth factors. This modulation ensures a controlled and balanced healing response. Through these mechanisms, FGF1 orchestrates the regeneration and restoration of corneal tissue following injury or surgery, promoting wound closure, re-endothelialization, and the formation of a functional corneal structure.
Unfortunately, several factors complicate corneal healing. Production of FGF1 in the eye goes relatively dormant after infancy, leaving low levels of the protein available in adult human aqueous humor, the fluid that bathes and supports the cornea. Native molecules of FGF1 are also highly unstable and have a short duration of biological activity. When oxidized, the proteins quickly unfold, losing their shape and their ability to bind with receptors on the surface of corneal cells. In cases where endothelial cells are already weakened by pre-existing conditions like Fuchs’ dystrophy or diabetes (or by excessive ultrasound required to remove advanced cataracts), the cornea is not always able to fully repair tissue damage inflicted by cataract surgery.
Although increasing the amount of FGF1 present in the eye could theoretically improve healing — and indeed, several other groups of researchers have explored therapeutic versions of the protein for use in dermal wounds — these efforts have been stymied by issues with the molecule’s stability. Given its propensity to break down, using the molecule to promote growth in the cornea would require near-daily injections into the eye, a procedure few patients would be willing to tolerate.
MODIFIED GROWTH FACTOR TTXH1114 CAN ACCELERATE CORNEAL HEALING
Trefoil Therapeutics is actively working toward improving outcomes for patients who experience poor vision because of corneal edema after cataract surgery. Its investigational therapy, TTHX1114, has been developed to stimulate natural cellular processes associated with native FGF1 that accelerate tissue healing and regeneration.
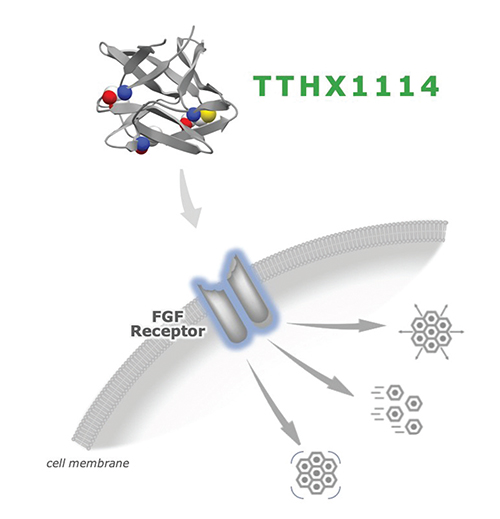
TTHX1114 is a modified version of FGF1 that binds to the same receptors on corneal cells, but has been engineered to be more durable, with enhanced persistence in the eye and improved binding capabilities to cell receptors. By mapping the three-dimensional structure of FGF1, Trefoil’s researchers were able to address identified weak points in the molecule, such as amino acids susceptible to oxidation. These amino acids have been replaced with similar structures that are less prone to oxidation. Trefoil has also improved the way the molecule folds, reducing the amount of free space available within its structure. By pushing its amino acids closer together, the protein effectively becomes tighter and more robust.
In addition to these improvements, Trefoil also inserted a new internal bond between two distant parts of the protein chain, locking the structure of TTHX1114 into place so that it cannot unfold. These changes greatly increase the overall stability of the protein, allowing it to remain in the eye long enough for effective receptor binding to create a therapeutic effect.
TTHX1114 retains all the natural functions of FGF1, including binding to tissue, regenerating cells after oxidative stress and other insults, and accelerating healing. Trefoil has demonstrated the potent protective and proliferative effects of TTHX1114 on corneal tissue in preclinical models and in human clinical trials.5
A BRIEF HISTORY OF TTHX1114
The scientific story behind the development of TTHX1114 stems from the exploration of factors that control the division and growth of corneal cells. Trefoil Therapeutics’ researchers built upon a large body of work that had established FGF1 as a critical factor in early development of the eye and cornea, setting up the pattern and promoting growth in the cornea and the eye overall.
Trefoil researchers sought to replicate this developmental environment in adult corneal tissue to promote growth, division, and tissue healing. FGF appeared to be a logical target in this context. The journey toward TTHX1114 involved building on previous work conducted in the lab of Ralph Bradshaw, a biochemist at the University of California, Irvine, who conducted pioneering work on nerve growth factors. Building from that work, Trefoil co-founder Mike Blaber — who is a former member of Bradshaw’s lab and Professor at Florida State University — made significant contributions to understanding the three-dimensional structure of FGF and its receptor binding properties.
In order to produce TTHX1114, Trefoil expresses the protein synthetically in E. coli via modifications in its amino acid sequence. The selection of specific amino acids to change required a comprehensive understanding of their impact on receptor binding and the physical stability of the molecule. Through years of research and experimentation, the team gained insights into altering the stability and affinity of FGF for the receptor. The design process involved careful selection of molecules from a library of variants, with further modifications guided by three-dimensional and free-energy modeling. A key focus was on preventing the unfolding of the protein, as its native structure was crucial for receptor interaction and preventing degradation. By fine-tuning the amino acid sequence, the team at Trefoil aims to ensure that TTHX1114 remains active in the biological environment for a long period of time and effectively interacts with corneal cells to facilitate tissue healing.
DELIVERY MECHANISMS FOR TTHX1114
Trefoil is currently developing two distinct delivery systems for this promising molecule. The first, an intracameral injection directly into the eye, targets endothelial cells on the back of the cornea, helping to improve recovery after surgeries that disturb or otherwise damage those tissues.
Phase 2 clinical trials of Trefoil’s intracameral injection have already shown promising results for patients undergoing a Descemet Stripping Only (DSO) procedure. This procedure is an alternative to corneal transplantation that does not require donor tissue and thus avoids the potential for graft rejection and the need for postoperative immunosuppression. In these cases, a single intracameral application of TTHX1114 led to recovery of vision to 20/40 in a mean time of 4.2 weeks following DSO.5 Trefoil researchers observed a significant dose-dependent effect of TTHX1114 on both the recovery of good vision and the deturgescence of central corneal thickness (CCT), with median CCT recovered to better than baseline by day 84.6 Restoration of corneal function and visual recovery indicated treatment with the drug accelerated healing through endothelial cell regeneration and migration.
In addition to its injectable form, Trefoil is also developing a topical solution of TTHX1114 that can treat epithelial cells on the cornea’s outer surface. Corneal epithelial defects are a hallmark of several conditions, including Sjogren’s syndrome, neurotrophic keratitis, and herpes virus infections.
Activation of herpes viruses, which cause oral and genital sores as well as chickenpox and shingles, for example, can lead to damage in the outer layer of the cornea. Ocular herpes (herpetic keratopathy) can produce corneal ulcers that blur vision and induce intense pain and inflammation — yet there are currently no treatments on the market used specifically for these ulcers.7 Trefoil’s topical formulation of TTHX1114 has been shown to reduce herpetic keratopathy and accelerate corneal ulcer wound healing by stimulating epithelial cell growth in preclinical models.
SUMMARY
In many cases, high-risk patients have few options for complication-free treatment of cataracts or other degenerative eye disorders. By filling this unmet need, TTHX1114 has the potential to significantly improve vision health, enhance the well-being of high-risk individuals, and alleviate economic burden on healthcare systems and economies. If successful, the drug could make it possible to effectively manage cataracts and corneal disease even in areas without easy access to surgical intervention — thus reducing visual impairment and restoring the quality of life for millions of individuals worldwide.
REFERENCES
- Wei Z, Hao C, Huangfu J, Srinivasagan R, Zhang X, Fan X. Aging lens epithelium is susceptible to ferroptosis. Free Radic Biol Med. 2021 May 1;167:94-108. doi: 10.1016/j.freeradbiomed.2021.02.010. Epub 2021 Mar 17. PMID: 33722625; PMCID: PMC8096685.
- Cicinelli MV, Buchan JC, Nicholson M, Varadaraj V, Khanna RC. Cataracts. Lancet. 2023 Feb 4;401(10374):377-389. doi: 10.1016/S0140-6736(22)01839-6. Epub 2022 Dec 21. PMID: 36565712.
- Rossi T, Romano MR, Iannetta D, Romano V, Gualdi L, D’Agostino I, Ripandelli G. Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021 Jan 13;6(1):e000464. doi: 10.1136/bmjophth-2020-000464. PMID: 33501377; PMCID: PMC7812090.
- Dixon SJ, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell. 2012 May 25;149(5):1060-72.
- Trefoil Therapeutics. “Trefoil Therapeutics Announces Positive TTHX1114 Phase 2 Study Data Showing Corneal Regeneration and Vision Recovery Following Descemet Stripping Only (DSO) Surgery,” September 29, 2022.
- Trefoil Therapeutics. “Trefoil Therapeutics’ Lead Investigational Candidate TTHX1114 Improves Rate of Visual Recovery after Descemet Stripping Only (DSO) in Phase 2 STORM Data Presented at ASCRS Annual Meeting,” May 10, 2023.
- Watson S, Cabrera-Aguas M, Khoo P. Common eye infections. Aust Prescr. 2018 Jun;41(3):67-72. doi: 10.18773/austprescr.2018.016. Epub 2018 Jun 1. PMID: 29922000; PMCID: PMC6003010.

Dr. David Eveleth is CEO of Trefoil Therapeutics. He has spent nearly 30 years in leadership positions at pharmaceutical and biotechnology companies, with a focus on ophthalmology and neuroscience. He has been involved in or led seven pharmaceutical INDs, the approval of several new drugs, and the approval of two medical devices. Prior to joining Trefoil, Eveleth led the Ophthalmology Medicines Development Group at Pfizer as vice president, a franchise that achieved peak revenue of $1.8 billion, and advised numerous biotechnology companies and venture capital groups. He earned his PhD in Biology from the University of California, Irvine.
Total Page Views: 1969