Issue:May 2022
REGENERATIVE MEDICINE - Delivering on the Promise of Regenerative Medicine in Type 1 Diabetes
INTRODUCTION
Each day is a challenge for the 1.4 million US adults and 200,000 youth under age 20 living with Type 1 diabetes (T1D).1,2 Their need to frequently monitor glucose (blood sugar) levels and adjust insulin doses to counter the effects of food, exercise, and physical and mental stress is often arduous and exhausting. In the US alone, 64,000 people are newly diagnosed with T1D each year, and that number is on the rise.2

Among youth under age 20, T1D cases increased by 21% between 2001 and 2009, while annual incidence rates increased by 1.9% from 2002 to 2015.3-5 An estimated 5 million people in the US are expected to have T1D by 2050, including nearly 600,000 youth.3 Moreover, the accompanying financial impact is significant: T1D-associated healthcare expenditures and lost income are estimated at $16 billion annually.4 Clearly, T1D represents a major public health problem in urgent need of solutions to better manage or cure the disease.
CHALLENGES OF LIVING WITH T1D
Since insulin was discovered in 1921, people with T1D have benefited significantly from advances such as faster-acting types of insulins, continuous glucose monitors, and automated insulin pumps. These tools have enabled less cumbersome, safer, and more physiologic insulin replacement and diabetes control. Unfortunately, most individuals with T1D still struggle with the challenges of managing their disease, including the need for multiple daytime glucose checks and frequent insulin dose adjustments to counter the effects of food, physical activity, and both physical and psychological stress on glucose levels. Moreover, because each day is different, insulin requirements vary from day to day.
Many individuals find it challenging to follow an intensive diabetes management regimen and therefore experience suboptimal glycemic control. When their diabetes is uncontrolled, patients are predisposed to acute consequences, such as severe hyperglycemia (high glucose), which can lead to compromised immune function, frequent urination, dehydration, vision problems, and other symptoms. In cases of missed or markedly inadequate insulin dosing, consequences can be more severe, leading to vomiting, acidosis, coma, or even death. When T1D is uncontrolled in the long-term, patients are at high risk for complications such as nerve damage, kidney injury and failure, vision loss, and amputations. They also have a three-fold greater likelihood of a heart attack or stroke compared to those individuals without T1D.
On the opposite end of the glucose spectrum, insulin also is commonly associated with hypoglycemia (low blood glucose levels), which also can be quite symptomatic, leading to coma, seizures, and death when levels fall severely low, and are unrecognized and untreated. Up to 40% of patients with T1D have hypoglycemia unawareness, meaning they become physiologically unaware of low glucose levels.6 Hypoglycemia unawareness is particularly concerning because these individuals have a six-to-seven-fold greater risk of experiencing a severe hypoglycemic event requiring assistance from others to bring glucose levels back to normal.
One large study found that 83% of people with T1D reported a hypoglycemic event within a 4-week period. Findings also showed a prospective rate of more than 73 hypoglycemic events/patient- year; 14.4% of patients experienced a severe hypoglycemic event with annual rate of 4.9 events/patient-year and a severe hypoglycemia hospitalization rate of 0.237 events/patient-year.7 Even more concerning are reports that as many as 4% to 10% of patients with T1D die of hypoglycemia.8
Although pancreas transplants can normalize glucose levels, these interventions subject patients to the risks of major surgery and require them to have lifelong immunosuppressive therapy. Moreover, these organs are in short supply. Patients with T1D are therefore in need of novel interventions that will provide a safe and effective alternative to current insulin replacement options. The field of regenerative medicine may well hold the key.
REGENERATIVE MEDICINE’S PROMISE
Insulin pumps and continuous glucose monitoring are helping improve the management of T1D but do not address the underlying biological driver of disease, namely the immune system’s attack on insulin-producing pancreatic beta cells. Clinical trials designed to non-selectively interrupt autoimmune attack on beta cells have proven unsuccessful when doses well-tolerated by patients are used that do not effectively suppress immune system attack.
Regenerative medicine, led by advances in stem cell research and biomaterials, has the potential to restore the body’s normal glucose regulatory system, offering promise in T1D treatment. These technologies, aimed at creating and implanting viable beta cells, could enable the tighter regulation of blood glucose levels. Once vascularized, these cells can monitor real-time glucose levels and rapidly adjust insulin delivery directly into the bloodstream versus patients injecting insulin into subcutaneous tissue, which can delay absorption. If successful, this mode of therapy could provide an adequate number of functioning beta cells to both prevent progression of any existing T1D complications and avoid treatment-associated hypoglycemia.
CADAVER ISLET CELL TRANSPLANT VIABILITY
Already, research has shown that islet cell transplants are a viable method of replacing the pancreas’ insulin-producing beta cells in addition to alpha and delta cells that are responsible for glucagon and somatostatin production, respectively. Transplanted cadaver-derived islet cells show promise in improving outcomes for patients with T1D, potentially providing better glycemic control, preventing severe hypoglycemia and offering relief from the need for multiple daily insulin injections or pump infusions.9
Between 1999 and 2015, more than 1,000 patients received greater than 2,000 allograft infusions of cadaver islets.10 About 90% of recipients were free of hypoglycemic events for more than 5 years, and more than 50% of recipients had sufficient allograft insulin production over the same period to preclude the need for exogenous insulin replacement.10 Despite these promising findings, however, only about 50% of transplant recipients achieve insulin independence at 1 year following completion of cell transplantation.10 Although transplantation using cadaver-derived islet cells has demonstrated proof-of-concept for islet cell replacement therapy, there is a limited supply of these donated cells. In addition, like pancreas transplants, cadaveric islet transplants still require chronic immunosuppression.
ADVANCING THE FIELD
Scientists are exploring regenerative medicine approaches to improve insulin replacement and potentially cure diabetes. Their work focuses on differentiating stem cell lines into pancreatic endodermal cells that enable implantation into patients and provide a nearly unlimited source of cells. Researchers also are investigating various cell and delivery engineering techniques aimed at ensuring long-term survival of transplanted cells. The goal is to develop a delivery device that can protect these cells from immune system attack while also enabling the exchange of glucose, hormones, and other biomolecules. Immune evasion is critical because if the device’s outer membrane is recognized as foreign, the body’s immune response will generate an inflammatory reaction leading to scarring that may impair adequate vascularization of the implanted cells, limiting insulin secretion.
Investigators are exploring several types of approaches, including a pouch-like device about the size of a credit card that encloses and protects the cells or a device that enables engraftment, as well as a method of individually coating islet cells with a protective polymer.11,12
PROMISING FINDINGS FOR ENDODERM CELLS
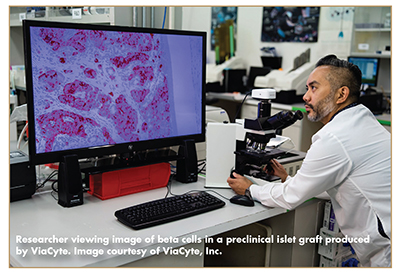
Restoring normal glucose regulation requires an adequate number of insulin-producing beta cells, as well as alpha cells that produce glucagon and prevents glucose levels from dropping too low. Toward that end, researchers are evaluating a variety of approaches focused on realizing the potential of regenerative medicine therapies for T1D. One approach uses pancreatic endodermal cells produced from stem cells that differentiate to become both alpha and beta cells. Promising preliminary data from a clinical study of this approach were reported by the company ViaCyte in June 2021 at the annual American Diabetes Association (ADA) meetings.13 In the study, subjects who were C-peptide negative at screening, indicating they were not producing insulin, received subcutaneous implants of encapsulated pancreatic endodermal stem cells.
Results from a Phase 2a clinical trial presented at ADA indicated that a patient was doing well with stimulated C-peptide levels up to 0.8 ng/mL (2.67 nmol/L) at 39 weeks.13 Investigators also reported a 0.8% reduction in HbA1c from a baseline of 7.4%, as well as increased time in desired glucose range from 54% to 88% at week 42 in this research subject.15 These results are promising, as C-peptide levels of >0.2 nmol/l become clinically meaningful, and clinicians consider >70% time-in-range to be an indicator of good diabetes control.14,15
FURTHER STEM-CELL RESEARCH
Other approaches using more mature pancreatic cells also are being evaluated in clinical trials. Vertex Pharmaceuticals, for example, launched a Phase 1/2 clinical trial using an islet product, immunosuppression, and intraportal cell delivery. Meanwhile, Seraxis has developed a stem cell islet product, likely to be delivered in a subcutaneous device, with plans to begin pilot clinical testing soon. Scientists are focused on determining the best method and location in which to deliver pancreatic cells, including various types of implanted devices and insulin release into patients’ portal veins to more directly inhibit hepatic glucose production. This work is also evaluating a variety of biomaterials and engineered cells that may eliminate the need for immunosuppressants. An example is CRISPR-based, gene-editing techniques, with the potential of developing stem cells engineered to evade immune system attack.16
BUILDING ON INNOVATION
Although regenerative medicine and stem cell-based therapies are an emerging field, preliminary data are promising and warrant further development of these innovations. Technological advances over the past 5 years have demonstrated insulin secretion associated with improved glucose regulation following implantation of pancreatic endodermal stem cells. Further advances in stem-cell engineering, immune-evasion technologies and vascularization of implanted cells have the potential to generate novel therapeutics that could lead to reduced treatment burden for patients with T1D and infuse new energy into efforts at finding a cure.
REFERENCES
- CDC National Diabetes Statistics Report, 2020.2Rogers, Kim C, Banerjee T, et al. Fluctuations in the incidence of type 1 diabetes in the United States from 2001 to 2015: a longitudinal study. 2017. BMC Medicine 15: 199. doi: 10.1186/s12916-017-0958-6.
- Rogers, Kim C, Banerjee T, et al. Fluctuations in the incidence of type 1 diabetes in the United States from 2001 to 2015: a longitudinal study. 2017. BMC Medicine 15: 199.Rogers, Kim C, Banerjee T, et al. Fluctuations in the incidence of type 1 diabetes in the United States from 2001 to 2015: a longitudinal study. 2017. BMC Medicine 15:199.
- Dabelea, Mayer-Davis E, Saydah E, et al. Dabelea, Mayer E, Saydah E, et al. Prevalence of Type 1 and Type 2 Diabetes Among Children and Adolescents From 2001 to 2009. 2014. JAMA 311: 1778-1786. doi: 10.1001/jama.2014.3201.
- ADA 2018. Economic Costs of Diabetes in the U.S. in 2017. Diab Care 41: 917-928. doi: 10.2337/dci18-0007.
- Divers J, Mayer-Davis EJ, Lawrence JM, et al. Trends in Incidence of Type 1 and Type 2 Diabetes Among Youths — Selected Counties and Indian Reservations, United States, 2002–2015. MMWR Morb Mortal Wkly Rep 2020;69:161-165.
- Martín-Timón I, del Cañizo-Gómez FJ. Mechanisms of hypoglycemia unawareness and implications in diabetic patients. World J Diabetes 2015;6(7): 912-926. doi: 10.4239/wjd.v6.i7.912.
- Khunti K, Alsifri S, Aronson R, et al. Rates and predictors of hypoglycemia in 27 585 people from 24 countries with insulin-treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obes Metab. 2016 Sep; 18(9): 907-915. doi: 10.1111/dom.12689.
- Cryer PE. Severe Hypoglycemia Predicts Mortality in Diabetes. Diabetes Care 2012 Sep; 35(9): 1814-1816. doi:10.2337/dc12-0749.
- Gamble A, Pepper AR, Bruni A, et al. The journey of islet cell transplantation and future development. Islets. 2018;10(2):80-94. doi:10.1080/19382014.2018.1428511.
- CITR Coordinating Center. Collaborative Islet Transplant Registry 10th Annual Report. Rockville, MD. 6 January 2017.
- Ernst AU, Bowers DT, Wang LH, et al. Nanotechnology in cell replacement therapies for type 1 diabetes. Adv Drug Deliv Rev. 2019;139:116-138. doi:10.1016/j.addr.2019.01.013.
- Battelino T, Danne T, Bergenstal RM, et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care. 2019;42(8):1593-1603. doi:10.2337/dci19-0028.
- Keymeulen B, et al. (2021) Stem Cell-Derived Islet Replacement Therapy (VC-02) Demonstrates Production of C-Peptide in Patients with Type 1 Diabetes (T1D) and Hypoglycemia Unawareness. American Diabetes Association’s Virtual 81st Scientific Sessions. Poster 196-LB.
- The DCCT Research Group: Effect of intensive therapy on residual β-cell function in patients with type I diabetes in the Diabetes Control and Complications Trial. Ann Intern Med 128:517 –523,1998. doi:10.7326/0003-4819-128-7-199804010-00001.
- American Diabetes Association, https://www.diabetes.org/healthy-living/devices-technology/cgm-time-in-range.
- Sluch VM, Swain D, Whipple W, et al. CRISPR-editing of hESCs allows for production of immune evasive cells capable of differentiation to pancreatic progenitors for future type 1 diabetes therapy. Abstract #9, European Association for the Study of Diabetes Virtual Meeting, Barcelona 2019.
Dr. Thomas Donner is the Director of The Johns Hopkins Diabetes Center. He has been a clinical investigator in numerous NIH- and industry-funded diabetes research trials. He was a co-PI in the NIH-funded Veterans Affairs Implantable Insulin Pump Study, a Co-PI on the NIDDK-funded Diabetes Control and Complications Trial/Epidemiology of Diabetes Intervention and Complications (DCCT/EDIC) Study, and Co-PI for the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D). He has served as a PI for TrialNet, a multicenter, international consortium of investigators studying ways to prevent Type 1 diabetes and preserve insulin secretion in individuals with newly diagnosed Type 1 diabetes. He has also served as PI for DEFEND-1 that used otelixizumab to try to prevent loss of islet cell function in new onset type 1 diabetes, and was a PI for a study involving the first subcutaneous implants of encapsulated pancreatic endodermal stem cells into patients with type 1 diabetes. Dr. Donner is currently collaborating with immunologists at Johns Hopkins on the characterization of a newly discovered immune cell that expresses both B and T cell receptors that may trigger type 1 diabetes.
Total Page Views: 4452










