Issue:September 2021
NASAL SPRAY BIOEQUIVALENCE - Between-Batch Bioequivalence (BBE): An Alternative Statistical Method to Assess In Vitro Bioequivalence of Nasal Product
INTRODUCTION
In the pharmaceutical industry, we can see the development of generics is significantly growing. This trend is mainly driven by countries to give patients easier access to drugs and to define regulations accordingly.
From an industrial perspective, the success of a generic product development is based on two elements: (1) compliance with all the regulatory requirements and (2) safety for patients (ie, has the same final therapeutic effect than the brand-name product).
One way to prove the equivalence, without long and expensive clinical trials, is to conduct in vitro bioequivalence evaluation between the Innovator (Reference product) and the proposed generic (Test product).
This evaluation is generally done through average bioequivalence (ABE) , or population bioequivalence (PBE) for in vivo and in vitro testing, through statistical methods.1-8 In vitro bioequivalence testing is not considered and evaluated in the same way by all instances taking part in the process.
Indeed, in the US FDA recommends the use of population bioequivalence (PBE), whereas Europe recommends using average bioequivalence (ABE).
While both ABE and PBE tests consider the device total variability, the between-batch variability, which is part of the total variability, is not considered individually in the mathematical definitions proposed by the FDA and EMA guidelines.
On one side, ABE only considers within-product variability. On the other side, the FDA guidance on Budesonide recommends to decompose the variance as a composite of a super-batch variability (ie, after pooling all batches per product) and the within-individual variability to study the life-stages (begin, middle, and end-of-use) equivalence.9
These calculation methods present some limits, particularly with high variable drug products [Coefficient Variation (CV%) greater than 29,6%] but not only. In practice, some limits of the classical methods may occur from 15% for within-Product CV%, where the power tests (ABE and PBE) drop off.
PBE is less permissive than ABE, if the Reference product variability is low. Conversely, PBE is more permissive than ABE if the Reference variability is high; even more so if the Test product variability is lower than the Reference product variability.
In order to prevent the risks of erroneously accepting equivalence in cases of high variability of the Reference, it is recommended to increase the number of samples in the goal to increase the power test on PBE and ABE calculations. This increases the confidence level of the bioequivalence conclusion.
However, this solution is undesirable from an industrial point of view since it increases costs and delays by inflating the number of tests to be carried out.
This increase in cost and associated delays is not aligned with the principle goal of reduced-cost generic medicines in a short time to market.
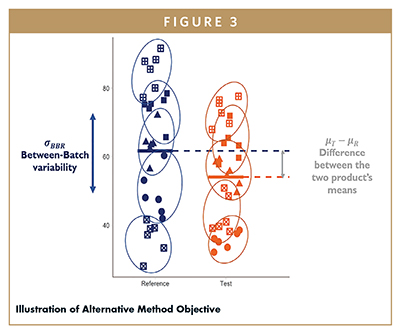
Considering this, an alternative statistical test, named between-batch equivalence (BBE), is proposed to assess in vitro bioequivalence. This statistical approach is based on the comparison between the mean difference (Reference − Test) and the Reference between-batch variability. The main hypothesis is that considering the between-batch variability of the Reference, the BBE test will be more appropriate to demonstrate equivalence in the case of variable drug products, without needing to increase the total required sample size. This statistical method can deal with normal scale data as well as after log transformation of the raw data.
METHOD – EXPERIMENTAL: SIMULATION
As reported in several studies, neglecting non-zero between-batch variability can have a strong impact on the bioequivalence conclusions.10,11 Thus, we developed a method that includes the Batch factor into the statistical equivalence test. In fact, the multiple measurements on a single batch induce a dependence between data and a violation of the independence assumption with the state-of-the-art methods ABE and PBE. The assumption of independence could be satisfied if the Batch factor is considered in the model.
Our methodology has been based on a comparison between the two population means (μT – μR) with the Between-Batch variability on the Reference drug product (sBBR).
As a first step, our study focused on the development of the statistical method, including an exact procedure to implement the test statistic and a confidence interval approximation to graphically illustrate the test results.18 Then, the type II error of the BBE method, ie, the FNR (False Negative Rate), was estimated by simulations and compared with the two mainly recognized statistical methods (ABE and PBE). In a second step, the type I error of the BBE method, ie, the FPR (False Positive Rate),18 was estimated by simulations to ensure that the BBE type I error remains of the theoretical order of 5%. In a third step, the BBE type II error was assessed and compared with the reference methods through a real case application on nasal spray in vitro performance that were performed on two Reference products from the market (which are by definition equivalent).
REAL CASE STUDY ON TWO NASAL SPRAY REFERENCE DRUG PRODUCTS
The BBE approach has been applied to two nasal sprays, Nasonex® (Merck) and Flonase® (GSK), which are corticosteroids used to treat nasal symptoms such as congestion, sneezing, and runny nose caused by seasonal or year-round allergies. These two products are already commercialized and considered individually as Reference products. In accordance with FDA guidance, two main parameters of in vitro spray performance were considered for the bioequivalence tests.12-14 The control of theses parameters ensures the quality of the nasal spray product and at the end the efficacy of patient treatment.
The statistical comparison of the three methods (ABE, PBE, and BBE) was performed separately on batches of Flonase and Nasonex products.
The aim was to evaluate whether the three methods can adequately conclude in an equivalence context of each product. For that purpose, the true positive rate of each method was estimated and compared. For both criteria (D50 and area) and both products (Nasonex and Flonase), batches of each product were randomly selected to be considered as a Reference or Test for the need of the bioequivalence evaluation.
The first, Dv50 (or D50) related to droplet size distribution (DSD), was measured by laser diffraction using a Spraytec (Malvern, UK) and an automatic actuator (Proveris, USA).15 Second, the spray pattern (area) was measured using a Sprayview system (Proveris, USA). This parameter, describing the shape of the spray is known for its high variability.16 The study has been performed at two distances (3 cm and 6 cm) as recommended in the guidance with an actuation speed of 80 mm/s.17
RESULTS
The results observed in the real case application confirm those observed in the simulation results. When the total variability of the Reference is low (around 5% for the DV50 criterion) the two state-of-the-art methods reached high true positive rates, with values greater than 99%. In this situation, the BBE equivalence test reached significantly lower true positive rates, depending on the between-batch variability (69% with πBB=25% and 84% with πBB = 43%). On the other hand, with the Area parameter, exhibiting higher variability on the Reference, 27% and 18% for the Flonase and Nasonex products, the BBE method showed higher true positive rates than ABE and PBE (70% versus 14% and 60% for the Flonase and 85% versus 62 and 69% for Nasonex).
CONCLUSIONS
The purpose of this work was to propose the development of an alternative statistical method to evaluate in-vitro equivalence. This alternative statistical method may be more appropriate to evaluate the in vitro bioequivalence for a nasal spray in a batch variability context with a reduced number of samples. Thus, BBE may be of particular interest to optimize the generic development in both in vitro and in vivo contexts.
REFERENCES
- European regulatory developments for orally inhaled and nasal drug products. Santos C, Marco G, Nagao L, Castro E, Chesworth T., AAPS PharmSciTech. 2018, https://pubmed.ncbi.nlm.nih.gov/30128799/.
- Bioequivalence requirements in the European Union: Critical discussion. García-Arieta A, Gordon J., AAPS J. 2012, https://pubmed.ncbi.nlm.nih.gov/22826032/.
- Performance of the population bioequivalence (PBE) statistical test using an IPAC-RS database of delivered dose from metered dose inhalers. Morgan B, Chen S, Christopher D, Långström G, Wiggenhorn C, Burmeister Getz E, et al. AAPS PharmSciTech. 2018, https://doi.org/10.1208/s12249-017-0941-8.
- Draft guidance: average, population, and individual approaches to establishing bioequivalence. FDA, CDER. 1999. https://www.fda.gov/files/drugs/published/Statistical-Information-from-the-June-1999-Draft-Guidance-and-Statistical-Information-for-In-Vitro-Bioequivalence-Data-Posted-on-August-18–1999.pdf.
- Regulatory considerations for approval of generic inhalation drug products in the US, EU, Brazil, China, and India. Lee SL, Saluja B, García-Arieta A, Santos GML, Li Y, Lu S, et al. AAPS J. 2015, Springer New York LLC, https://doi.org/10.1208/s12248-015-9787-8.
- Draft guidance on budesonide [Internet]. US Food and Drug administration, 2016, http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM319977.pdf.
- Draft guidance on budesonide [Internet]. US Food and Drug administration, 2016, http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM319977.pdf.
- Draft guidance on mometasone furoate monohydrate. US Food and Drug Administration. 2019, https://www.accessdata.fda.gov/drugsatfda_docs/psg/Mometasone_furoate_nasal_spray_NDA_020762_RV_02-2019.pdf.
- Method for testing bioequivalence of a distribution device. Liandrat S, Petitcolas C, Jonathan B. France. 2020, https://patentscope.wipo.int/search/en/detail.jsf?docId=WO2020053223.
- Performance properties of the population bioequivalence approach for in vitro delivered dose for orally inhaled respiratory products. Morgan B, Strickland H. AAPS J. 2014, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3889535/.
- Between-batch pharmacokinetic variability inflates type I error rate in conventional bioequivalence trials: a randomized Advair Diskus clinical trial. Burmeister Getz E, Carroll KJ, Mielke J, Benet LZ, Jones B. Clin Pharmacol Ther Nature Publishing Group. 2017, https://pubmed.ncbi.nlm.nih.gov/27727445/.
- Draft guidance on fluticasone propionate. US Food and Drug Administration. 2019, https://www.accessdata.fda.gov/drugsatfda_docs/psg/Fluticasone_propionate_nasal_spray_NDA_020121_RV_02-2019.pdf.
- Draft guidance on mometasone furoate monohydrate. US Food and Drug Administration. 2019, https://www.accessdata.fda.gov/drugsatfda_docs/psg/Mometasone_furoate_nasal_spray_NDA_020762_RV_02-2019.pdf.
- High resolution visualization and analysis of nasal spray drug delivery. Inthavong K, Fung MC, Tong X, Yang W, Tu J. Pharm Res. 2014, https://doi.org/10.1007/s11095-013-1294-y.
- Analytical challenges of spray pattern method development for purposes of in vitro bioequivalence testing in the case of a nasal spray product. Grmas J, Rok D, Rade I. Aerosol Med Pulm Drug Deliv. 2019, https://pubmed.ncbi.nlm.nih.gov/30964389/.
- Performance of the population bioequivalence (PBE) statistical test with impactor sized mass data. Chen S, Morgan B, Beresford H, Burmeister Getz E, Christopher D, Långström G, et al. AAPS PharmSciTech AAPS PharmSciTech; 2019, https://pubmed.ncbi.nlm.nih.gov/31444601/.
- Bioavailability and bioequivalence studies for nasal aerosols and nasal sprays for local action [Internet]. US Food and Drug Administration. 2003, http://www.fda.gov/cder/guidance/index.htm.
- Between-Batch Bioequivalence (BBE): a Statistical Test to Evaluate In Vitro Bioequivalence Considering the Between-Batch Variability. Bodin J, Liandrat S, Kocevar G, Petitcolas C. AAPS J, 2020. https://doi.org/10.1208/s12248-020-00486-5.

Céline Petitcolas is Customer Technical Support for nasal range at Nemera. Holding a Materials Engineering degree from the École Nationale Supérieure de Chimie et de Physique in Bordeaux, France, she joined Nemera in 2012 to develop pharmaceutical devices, focusing especially on the nasal spray area. Her role consists in helping and assisting customers from a technical point of view in their development of nasal sprays and more specifically in the area of bioequivalence. She is the preferred technical contact for customers as she interfaces with multiple Nemera teams (marketing, sales, technical) to bring customers and partners the support they need.

Manuela Basso is an experienced communications professional, with a journalism and marketing background. She holds a European Master in Management and specializes in International Marketing. After various experiences in different fields, she has been working at Nemera for 6 years, developing effective communications to support Nemera’s overall vision and mission: to put patients first.
Total Page Views: 7663