Issue:November/December 2021
INHALATION THERAPY - An Overview to Drug-Nebulizer Combination Development With Biologics
BENEFITS OF INHALATION THERAPY FOR DELIVERY OF BIOLOGICS
Biologic drugs have been shown to provide great contribution to the treatment of several rare diseases in the past few years. When looking at the number of new drugs approved by the US FDA, biologics have accounted for approximately 27% of new approvals since 2014.1 Although their administration is traditionally performed via intravenous injections, research has revealed that for the treatment of diseases that affect the respiratory airways, more specifically the lower airways, direct administration for topical delivery through inhalation has presented itself as a more suitable approach.
Two of the major benefits of inhalation therapy to support the delivery of biologics are the reduction of potential systemic side effects and the need for lower doses to achieve therapeutic effect. Currently, the most common route of administration, intravenous administration, has been reported to increase systemic exposure of different parts of the body to the biologic components, hence only allowing a small amount of the initially injected drug to reach the lungs. Conversely, inhalation therapy has demonstrated that by directly delivering biologic drugs into the lungs, active pharmaceutical ingredients can be successfully uptaken via topical delivery and further avoid systemic circulation. Moreover, while clearance of biologic components from the lungs mostly takes about 24 hours, plasma half-lives of antibodies may be clear only after 21 days or longer.2
In recent years, biologic drugs are increasingly being investigated for delivery with inhalation therapy, which has initiated more in-depth discussions about the implications of formulation development and their pairing with adequate inhaled devices for more efficient treatment outcomes.
IMPLICATIONS OF DEVICE SELECTION TO DELIVER BIOLOGICS
Biologic drugs are particularly susceptible to several factors, such as high temperature, shear forces, and extreme pH, which may lead to the denaturation of their structure or result in aggregation. Due to the aforementioned nature of biologic drugs, selecting the most suitable delivery system is vital to ensure that the functionality of the drug remains highly active when reaching the airways to effectively treat respiratory diseases.
The additional processing required to administer biologic drugs via dry powder inhalers (DPIs), which may require the formulation to be freeze or spray dried, exposes the biologic drugs to extreme conditions that can easily lead to their degradation. On the other hand, metered dose inhalers (MDIs), which permit the formulation to be in the liquid state, may also degrade the structure of proteins by allowing them to be in a liquid environment for extended periods of time and in contact with hydrofluoroalkane (HFA) propellants further risking their integrity. Although in recent years it has been possible to overcome some of the issues previously mentioned, the large doses required to reach therapeutic treatment may also lead to disregard DPIs and MDIs when selecting a fitting device, leaving nebulizers as the most suitable delivery system.3
Nebulizers, devices that transform liquid medication into aerosol, are usually divided in three categories: jet, ultrasonic, and mesh nebulizers. The formerly developed jet nebulizers operate by generating aerosol by the means of pushing air pressure into a container filled with liquid medication. The shear forces produced during this process are highly detrimental to biologic drugs that can readily aggregate during the aerosolization process. Similarly, the heat generated by ultrasonic nebulizers that produce aerosol with ultrasonic waves, which are driven by a piezoelectric component, can also lead to denaturation of biologics, making them inactive. Only the newest type of nebulizers, mesh nebulizers, have been shown to provide one of the most adequate mechanisms for the delivery of biologics, with low shear forces and heat generation.4
As a result of this scenario, several of the new developments involving inhaled biologics are in combination with mesh nebulizers, covering indications ranging from asthma and chronic obstructive pulmonary disease (COPD) to cystic fibrosis and non-cystic fibrosis bronchiectasis.
FORMULATION CHARACTERISTICS & THEIR EFFECT ON AEROSOL CHARACTERIZATION
One of the key elements for the successful delivery of biologics is the selection of excipients. The addition of excipients can help protect the structure of biologic compounds, and subsequently aid them to retain their stability and activity in aqueous solutions and even after nebulization. Unfortunately, when it comes to inhaled biologics, the number of approved inhaled excipients by the US FDA remains limited.5 Surfactants, such as polysorbate, as well as sodium chloride and arginine, are commonly used in biologic formulations to regulate the physicochemical characteristics that will later influence the aerosol characterization when in combination with nebulizers.
To achieve desired aerosol characteristics and target high lung deposition, some of the main properties that are related to aerosolization of the liquid medication are viscosity, surface tension, and osmolality. Several biologic formulations tend to present higher levels of viscosity, especially at high concentrations. This factor is commonly associated to lower output rate of aerosol generation, resulting in longer nebulization time. Viscosity-reducing excipients, such as lysine and arginine, can be added to the biologic formulation to increase output rate, which has been described as an effective way to improve patient adherence by reducing nebulization time.6 Other frequently used excipients that have been found to stabilize biologic formulations are buffers containing sodium chloride, hydrochloric acid, citric acid, among others, by positively adjusting and maintaining the pH value of the formulations.
In a similar fashion, incorporation of polysorbates can decrease surface tension and at the same time stabilize biologic formulations by preventing aggregation. Nonetheless, it has been stated that lower surface tension results in lower output rate for mesh nebulizers, which can typically aerosolize solutions in the range of 35-75 mN/m (Figure 1).7 Finally, the use of certain excipients has also been linked to causing coughing response in patients receiving their inhalation treatment due to stimulation of the transient receptors in the airway afferent nerves.8
NEBULIZER CUSTOMIZATION & DRUG-DEVICE CO-DEVELOPMENT
In addition to the formulation tailoring alternatives to deliver biologics, mesh nebulizers also offer customization solutions that are increasingly becoming a new trend for the development of drug-device combination products. Adjustments in the hardware and software of the devices intend to satisfy the requirements to effectively deliver biologic drugs without affecting their properties. Accounting as one of the fundamental factors in the customization of these devices is the mesh membrane itself. Mesh membranes can vary based on different aspects of their composition, such as material, formation mechanism, pore size and structure, thickness of the membrane, and pitch. The combination of these aspects generates a vast number of alternatives to fit formulation characteristics. Similarly, modifications on the mesh driving power and frequency derived from the firmware can further support the delivery of highly viscous biologic drugs or those with lower surface tension induced by polysorbates.
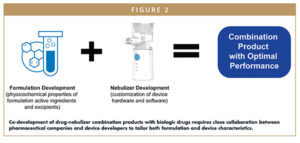
Hence, co-development of a drug-nebulizer combination product may attain higher levels of success when knowledge from both formulation and device side are integrated to develop a combination product in which aspect of the two parts are adjusted to achieve the desired outcome (Figure 2). Then fluid communication between the teams becomes an essential aspect to address issues at an early stage of the feasibility studies, avoiding potential setbacks in the subsequent steps of the development process.
NEW FEATURES TO ENHANCE BIOLOGICS DELIVERY EFFICIENCY
Due to the higher cost of biologic drugs, one of the principal objectives when nebulizing these drugs is to reach elevated levels of active pharmaceutical ingredients being delivered to the respiratory airways. Most mesh nebulizers operate under a continuous-output mode; however, new technologies have been incorporated to these devices to switch to a mode in which aerosolization only takes place during a fraction of the inhalation cycle, thus reducing the amount of aerosol otherwise wasted during exhalation.9 This mechanism called breath actuation is in many cases the preferable solution in the development of novel drug-nebulizer combination products.
Breath actuation can be incorporated to the nebulizer relying on different mechanisms, which can be either mechanical or electronic, with pressure sensors being one of the most widely applied technologies. Restricting aerosol formation during a specific fraction of the breathing cycle, does not only allow to increase the delivered dose, but also greatly reduces the amount of aerosol wasted in the environment during exhalation as well as the potential expulsion of aerosol that is not fully deposited into the lungs. This type of aerosol that is known as fugitive emission has been labelled as hazardous for people surrounding those receiving their inhalation treatment, resulting in an additional reason to prevent their excessive formation.10
Another feature with rapidly increasing demand in the inhalation field is connectivity. In recent years, connectivity has become the top choice for inhalers and nebulizers, aiming to monitor and improve patient adherence.11 Biologic drugs in combination products with nebulizers are also expected to move toward this trend as it will help better assess the efficacy of drugs either in clinical trials or later during commercialization. Creating a connected environment between physicians, nurses, caregivers, and patients would allow to closely follow the treatment of different diseases, monitor the patient’s evolution, and improve the expected outcome even when the treatment is performed remotely from home. Due to the involvement of personal and private information, the development of these networks comes along with security risks that should be addressed under specific regulations to guarantee the protection of patients’ private data at all times. Several regulations and guidelines are already in place, including the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR).12
SUMMARY
As novel therapies continue to be developed with the advancement of biologic treatments, new approaches in the inhalation therapy field, concerning to proteins, peptides, and nucleic acids, are also projected to continue to grow. At the current time, mesh nebulizers are positioned as one of the top systems to deliver these formulations. The final realization of these projects will ultimately depend on the integration for co-development between pharmaceutical companies and devices developers to bring together new treatment options for common and rare diseases. Moreover, the incorporation of new features, such as connectivity and breath actuation, will continue to add value to the development of biologic-nebulizer combination products by ensuring high levels of drug delivery and a well-structured and secure network to monitor and improve patient adherence.
REFERENCES
- Torre, B.G. & Albericio, F. (2021). The Pharmaceutical Industry in 2020. An Analysis of FDA Drug Approvals from the Perspective of Molecules. Molecules, 26(3), 627. https://doi.org/10.3390/molecules26030627.
- Koussoroplis, S. J., Paulissen, G., Tyteca, D., Goldansaz, H., Todoroff, J., Barilly, C., Uyttenhove, C., Van Snick, J., Cataldo, D., & Vanbever, R. (2014). PEGylation of antibody fragments greatly increases their local residence time following delivery to the respiratory tract. Journal of controlled release : official journal of the Controlled Release Society, 187, 91–100. https://doi.org/10.1016/j.jconrel.2014.05.
- Respaud, R., Marchand, D., Parent, C., Pelat, T., Thullier, P., Tournamille, J. F., Viaud-Massuard, M. C., Diot, P., Si-Tahar, M., Vecellio, L., & Heuzé-Vourc’h, N. (2014). Effect of formulation on the stability and aerosol performance of a nebulized antibody. mAbs, 6(5), 1347–1355. https://doi.org/10.4161/mabs.29938.
- Pritchard, J. N., Hatley, R. H., Denyer, J., & Hollen, D. V. (2018). Mesh nebulizers have become the first choice for new nebulized pharmaceutical drug developments. Therapeutic delivery, 9(2), 121–136. https://doi.org/10.4155/tde-2017-0102.
- Bodier-Montagutelli, E., Mayor, A., Vecellio, L., Respaud, R., & Heuzé-Vourc’h, N. (2018). Designing inhaled protein therapeutics for topical lung delivery: what are the next steps?. Expert opinion on drug delivery, 15(8), 729–736. https://doi.org/10.1080/17425247.2018.1503251.
- Beck-Broichsitter M. (2019). Making Concentrated Antibody Formulations Accessible for Vibrating-Mesh Nebulization. Journal of pharmaceutical sciences, 108(8), 2588–2592. https://doi.org/10.1016/j.xphs.2019.03.009.
- Pritchard J. N. (2017). Nebulized drug delivery in respiratory medicine: what does the future hold?. Therapeutic delivery, 8(6), 391–399. https://doi.org/10.4155/tde-2017-0015.
- Chang, R., Kwok, P., Ghassabian, S., Brannan, J. D., Koskela, H. O., & Chan, H. K. (2020). Cough as an adverse effect on inhalation pharmaceutical products. British journal of pharmacology, 177(18), 4096–4112. https://doi.org/10.1111/bph.15197.
- Arunthari, V., Bruinsma, R. S., Lee, A. S., & Johnson, M. M. (2012). A prospective, comparative trial of standard and breath-actuated nebulizer: efficacy, safety, and satisfaction. Respiratory care, 57(8), 1242–1247. https://doi.org/10.4187/respcare.01450.
- McGrath, J. A., O’Sullivan, A., Bennett, G., O’Toole, C., Joyce, M., Byrne, M. A., & MacLoughlin, R. (2019). Investigation of the Quantity of Exhaled Aerosols Released into the Environment during Nebulisation. Pharmaceutics, 11(2), 75. https://doi.org/10.3390/pharmaceutics11020075.
- Denyer J. (2010). Adherence monitoring in drug delivery. Expert opinion on drug delivery, 7(10), 1127–1131. https://doi.org/10.1517/17425247.2010.517520.
- Phillips M. (2018). International data-sharing norms: from the OECD to the General Data Protection Regulation (GDPR). Human genetics, 137(8), 575–582. https://doi.org/10.1007/s00439-018-1919-7.
To view this issue and all back issues online, please visit www.drug-dev.com.

Hernan Cuevas Brun is Marketing Manager at HCmed Innovations. He has more than 7 years of experience in the drug delivery field, holding a BS in Biomedical Engineering and a Master’s in Business Administration. He is responsible for the market positioning of HCmed’s nebulizers, supporting the development of drug-nebulizer combination products with pharmaceutical companies, while also coordinating the products’ branding and assisting with business development projects. Moreover, he is involved in the development of connected devices, supporting the company’s programs and establishing alliances with new partners to expand into digital health.
Total Page Views: 7961