Issue:April 2021
INHALATION DELIVERY - Inhaled Drug Development: Optimizing Delivery
INTRODUCTION
When developing a drug to be administered through an inhaled route, there are many factors to take into account, some or all of which may change as the development program moves toward commercialization. No two development programs for inhaled drug products will be driven by the same factors; any new product concept, therefore, needs to be approached with a fresh mindset and without preconceptions or bias ideally in terms of the delivery technology or device. There also needs to be a recognition that as the program progresses, there may be a requirement to adapt the strategy as each new phase is reached in the journey from early phase development through scale-up to commercialization. Although retaining the same delivery platform throughout the entire process might be the preferred option, it may be necessary to switch from the one used in the earlier stages of development, even up to proof-of-concept, to the one that ultimately might be commercialized.
One of the first major considerations in choosing a delivery technology will be the physical properties of the active pharmaceutical ingredient (API): whether it is a small molecule API or a biologic; whether it is readily solubilized; and the likely dose range. Cost is also a significant factor in the early development stage – not only the cost and availability of the API, but also the cost of any device and the likely volumes involved.
Additionally, there are strategic issues that need to be borne in mind, including the development strategy being employed, and the nature of the client or development partner and their need for early value inflexion on clinical proof-of-concept. A new chemical entity (NCE) typically has an uncertain future, putting the emphasis on successful proof-of-concept studies and the need for dosing flexibility, speed, and cost management.
As one method of delivery, using a smart nebulizer can be a very effective way of developing a product to the early clinical stage. This technology platform can quickly maximize lung deposition consistently from patient to patient with a simple and straightforward formulation development process, consuming minimal drug material to get the best probability of success.
DEVELOPMENTAL CONSTRAINTS
In one project, for example, an innovator company was developing a highly water-soluble small molecule to target deep and very high lung deposition. The molecule was in the higher dose range, making it potentially less amenable to being formulated as a dry powder inhaler (DPI), although a capsule format might also have been suitable. Aimed at treating a niche disease, it required consistent dosing from patient to patient with a simple formulation development process. The more drug that could be dosed to the lungs and the more reproducibility that was achieved, the better the chances of a positive outcome.
A hand-held mesh nebulizer was chosen as it allowed all of the pre-Phase 1 clinical study pharmaceutical development work to be completed with only a small quantity of material (100 g). This was sufficient to conduct all of the formulation development work and analytical method development, as well as phase-appropriate validation, stability testing, and product performance characterization studies. Only as much drug was dissolved as was required for the immediate testing, meaning that expensive and scarce API was not wasted during early development.
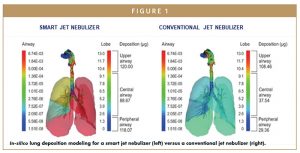
In-silico lung deposition modeling studies showed that smart jet nebulizers were more effective than conventional jet nebulizers in terms of lung deposition, and also significantly better than a high-performing DPI (Figure 1). The figure shows that twice as much drug was deposited in the central airways compared with the conventional system, and almost four times as much in the smaller airways. A smart nebulizer approach also offered the potential for more consistent delivery because the patient was guided to take every breath in the same way by the device. In the mesh nebulizer system, the dose sat on top of the mesh and typically more than 90% percent of the dose was delivered to the patient. A further advantage of smart nebulization is its ability to deliver a variety of different clinical doses through only two solution strengths by dispensing different volumes into the nebulizer. In this case, the development program resulted in a clinic-ready product in only 18 months.
MANUFACTURING CONSIDERATIONS
In early development phases of any project, there is an inevitable trade-off between the scale of manufacture and the number of batches that can be produced to build scientific understanding. However, one of the keys to successful development is an assurance of the ability to scale-up the manufacturing processes. Drug product development in the respiratory field, where reliable scale-up can be difficult to achieve, presents the challenge of deciding what constitutes an appropriate scale at each stage of development.
Minimizing the risks associated with the scale-up of manufacturing processes is vital to developing successful products, and so the choice of equipment is important to be able to move seamlessly from laboratory scale to commercially representative scale during the development and, ultimately, commercial-scale filling equipment.
SCALE UP VALIDATION
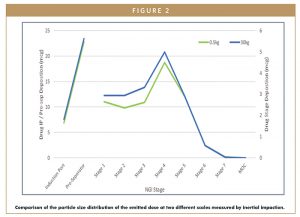
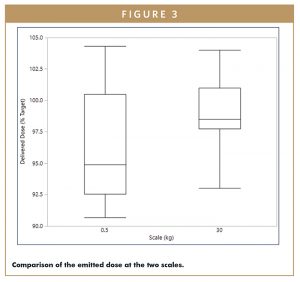
In a project to develop a generic DPI treatment for asthma and chronic obstructive pulmonary disease (COPD), a blend scale-up model was validated to demonstrate that it was possible to achieve comparable drug product performance from batches made at 500-g laboratory blend scale and batches made at 30-kg commercial blend scale (Figures 2 & 3). Figure 2 gives a comparison of the particle size distribution of the emitted dose for the two different scales, and Figure 3 gives a comparison of the emitted dose at the two different scales.
This model enabled a significant amount of the development work to be conducted in the laboratory at development scale, minimizing material costs and enabling faster execution of experiments, but also gave confidence in the ability to move to the larger scale at a later date. This assurance also meant that capital investment at the commercial manufacturing site could be made at a later development stage, based on a risk-based approach for this project.
PATIENT NEEDS
Whatever delivery platform is chosen for the final product, it must be suitable not only from the point of view of design and manufacturing, but also from the perspective of the needs of the target patient population, taking into account age range, any dexterity or cognitive issues that could affect usability and compliance, lifestyle, and patient expectations based on other available devices.
Other considerations should include the nature of the disease, whether the therapy will be delivered at home or in hospital, whether delivery needs to be to the deep lung or the central airways, and the number of doses per day.
PHASE-APPROPRIATE DEVELOPMENT
The initial choice of a platform may not necessarily be appropriate for every stage of a development program. Ideally, a development project would yield a well-characterized, commercially ready device, and a process and formulation at the pivotal clinical stages of development. However, in reality, it is not until a commercial process has been established, and many batches manufactured and tens or hundreds of thousands of devices delivered into the hands of patients, that a fuller understanding of the product is achieved. It is therefore important to approach defining the target delivery technology in a “device agnostic” manner, without being influenced by previous programs or a technology bias towards a particular platform.
ENSURING SUCCESS
Success of a program at the commercial stage is defined by a range of elements. Clearly, maximizing volumes and increasing access to patients requires being in a position to roll out a product in as many geographies in which it can be approved. It is vital for commercial success to maximize volumes and capacity, yields, process capability, efficiencies through synergies and economies of scale, and to have the greatest supply chain flexibility while minimizing risk, obsolescence, cycle times, downtime, costs, and working capital. It is also essential to eliminate redundancy, waste, and excess inventory over time. Maximizing volumes can also provide opportunities to reduce costs and help maintain a positive margin position even in adverse or competitive pricing environments.
A global supply chain and procurement function is therefore key within any development company, giving it the ability to manage the forecasting, logistics, cost management, contractual, and business continuity elements. It must also ensure effective management of inventory, including safety stock, and distribution to its clients and ultimately to patients. This discipline and experience brings great value when managing situations that threaten to disrupt supply of critical medicines.
Ongoing assessment and evaluation in the commercial phase will enable the product to evolve, grow, and maximize its potential through focused continuous improvement. Feeding the know-how and experience acquired in this phase back to development teams will aid industrialization, minimize cost-of-goods, and build robustness into future products.
Significant experience in all stages of the development life cycle, and applying the best technology solutions at each stage, can help organizations to successfully take an inhaled development program from feasibility through development and on to commercialization.
Selecting the delivery device or technology platform on the basis not only of the needs of the patient and the nature of the disease, but also on opportunities for accelerating the proof-of-concept or early clinical stages by using fast-to-clinic approaches can help to accelerate the project through later-stage development by combining the approach with seamless scalability, designing in manufacturability, and choosing an appropriate manufacturing strategy.

Dr. Sandy Munro is Vice President – Pharmaceutical Development at Vectura. He has been with Vectura since 2008 and is responsible for the company’s new technology development and also for product development programs utilizing Vectura’s smart nebulizer devices.

Nikki Willis is Vice President – Pharmaceutical Development at Vectura. She has worked in inhaled product development for over 30 years, and leads Vectura’s pharmaceutical development department, responsible for dry powder inhaler (DPI) product development programs.

Dr. Geraldine Venthoye is Executive Vice President – Product Development at Vectura, where she leads Vectura’s Pharmaceutical Development and Medical Device Development departments, and is responsible for the strategic and technical advancement of the company’s products, development services and technology platforms.
Total Page Views: 5015