Issue:October 2020
IMMUNOGENICITY TESTING - Regulatory Updates for Immunogenicity Assessment of Therapeutic Proteins
INTRODUCTION
Immunogenicity assessment is a significant challenge in the development of therapeutic proteins, such as monoclonal antibodies, recombinant proteins, antibody-drug conjugates, and fusion proteins. Due to high molecular weight, complex structure, and post-translational modifications, biologics have high potential to illicit anti-drug antibodies (ADA) responses. Developing adequate strategies for immunogenicity evaluation is therefore crucial for preclinical and clinical development of biologics programs. These ADAs — whether neutralizing antibodies (NAbs) that block efficacy of a protein by targeting domains critical for function or non-neutralizing antibodies — can have significant consequences, affecting a product’s pharmacokinetics (PK), pharmacodynamics (PD), drug efficacy, and safety.1
In early 2019, the FDA updated its guidelines for immunogenicity testing and recommended a risk-based approach to evaluating and managing immune responses elicited by therapeutic proteins. Timing and extent of developing, validating, and implementing ADA assays during the drug development stage are dependent on the risk assessment of the product.
The following provides a high-level analysis of the significant changes to the guidance compared to the immunogenicity draft guidance released in 2016, and the implications for drug development programs.
WHAT’S DIFFERENT IN THE 2019 GUIDANCE?
The significant revisions focus on the following areas:
-Risk assessment and timing on validating assays
-Statistical approaches to determine cutpoint
-Removal of the long-term stability requirement
-Development of assays to measure neutralizing antibodies
-Strategies for managing pre-existing antibodies
-Updates in documentation requirements.
RISK ASSESSMENT UPDATES
In the 2019 guidance, the FDA revised its recommendations on immunogenicity risk assessment, stating that a risk assessment and a rationale for testing should be submitted in conjunction with the investigational new drug (IND) application. Previously, the FDA advised that sponsors should provide a rationale for immunogenicity testing rather than the risk assessment itself.
The risk assessment encompasses specific analyses and discussions on therapeutic protein factors that would influence its immunogenicity, including discussions on the drug product itself (eg, if it has an endogenous counterpart) and how likely a subject population is to respond to exposure to the therapeutic protein (eg, cancer patients who are often immune-compromised may mount a lower immune response to a protein, whereas people with autoimmune disorders would be more likely to develop immune responses).
In considering a risk assessment, sponsors should also examine the attributes of a product that may influence immunogenicity. Product-related factors that may contribute to immunogenicity include:
-Whether the product origin is human or foreign
-Novel structural formats, such as fusion proteins, bispecific antibodies, and other engineered antibodies
-Post-translational modifications
-The tendency of a therapeutic protein to aggregate
-Glycosylation or PEGylation
-The presence of impurities with adjuvant activity.
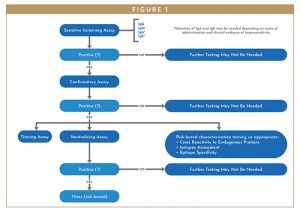
With respect to assay design, the FDA lays out a multi-tiered approach (Figure 1) for testing therapeutic proteins.1 The approach consists of a sensitive screening assay for ADA followed by a confirmatory assay for any positive results. The FDA recommends that biologic drugs that cause a confirmed ADA assay result should undergo testing for neutralizing antibodies. Titer, isotype and domain specificity of the ADA may also be assessed along with PK, PD and clinical outcome evaluation.
STATISTICAL APPROACH TO DETERMINING CUT-POINT UPDATES
The cut-point of the assay determines whether the sample response is positive or negative; FDA suggests a cut-point having false-positive rate of approximately 5% is desirable for the initial screening assay because it maximizes detection of true positives, which is important for ensuring the adequate subjects who may develop antibodies to a therapeutic protein to be identified.
Historically, the assay cut-point was determined directly from a normal percentile, which assumes that distribution of results will follow a traditional bell-shaped curve. This method is simple, but it significantly underestimates the false positive rate, which results in a lower chance of satisfying the 5% false positive rate. For example, the traditional method for a screen assay is estimated to produce a cut-point only having less than 50% chance to satisfy the required 5% false positive rate.2
In the 2019 FDA guidance, the FDA requires sponsors to find a statistically sound method to determine the cut-point, whereas previous guidance documents stated that cut-point estimation could be achieved with a small number of samples. The 2019 guidance offers an approach wherein a screening assay should have at least 90% chance to satisfy the 5% false positive rate, and a confirmatory assay should have at least 80% chance to satisfy the 1% false positive rate. The assay sensitivity can be calculated by interpolating the linear portion of the dilution curve to the assay cut-point. And low positive control, as an important system suitability control, should be set at a level that is consistently above the cut-point with a targeted 1% of failure rate. Statistical analysis can add value in determination of assay sensitivity and low positive control.
There is no generally accepted standard method for these statistical determinations. One way is a statistically sound estimation package, including outlier exclusion and cut-point estimation satisfying the new FDA requirements. The statistical methodology is based on order statistics, Bayesian, and Monte Carlo methods and can be applied to any assay data given that there are at least 50 samples. These methods are designed to satisfy or exceed the FDA confidence requirements without being too conservative. The required computations have been implemented using standard statistical programming languages SAS and R.
REMOVAL OF LONG-TERM STABILITY REQUIREMENT
Regarding sample stability, an important update in the 2019 guidance is that the expectation on long-term storage stability of positive control antibodies is now removed. Antibodies are known to be stable for at least two years when stored at -20°C or below, and evaluation of the positive control antibodies, which are essentially surrogate antibodies, for extended storage in deep freezers does not add value to the understanding of the ADA sample stability. The guidance now advises that sponsors minimize freeze-thaw cycles by appropriately aliquoting subjects’ samples and evaluating short-term stability, including, as relevant, freeze-thaw cycle and refrigerator-and room-temperature stability of positive control antibodies. The agency, however, removed the wording on assessment of long-term stability.1
MINIMAL REQUIRED DILUTION
Matrix components, such as serum, saliva, or plasma, are known to interfere with assay selectivity, contributing to nonspecific signals and potentially obscuring positive results. Therefore, the FDA notes the frequent need to dilute subject samples to ensure the ability to detect ADA. The FDA 2019 guidance allows sponsors to use one of three definitions of the minimal required dilution – either the sample dilution that yields to highest signal-to-noise ratio, the sample dilution that results in a signal closest to assay diluent, or the sample dilution that results in the highest signal to variability ratio.3 The expansion of definitions allows sponsors more options to better achieve optimal selectivity for an assay.
NEUTRALIZING ANTIBODIES
If immunogenicity testing finds and confirms positive ADAs, the FDA guides that sponsors should assess for NAbs. NAbs can have significant impact on drug PK, PD, safety, and efficacy, and the overall impact of antidrug antibodies may correlate with the activity of NAbs; however, designing appropriate assays for their detection is quite challenging as the traditional guide for developing the Nab strategy has been the risk of immunogenicity to patient safety.5 The FDA has made extensive updates to its guidance for assays on neutralizing antibody action as the science has evolved.
One update is increased flexibility from the FDA for the format of assay that can be used to assess NAbs, and the guidance notes that selection of the assay format depends on various factors, such as the mechanism of action of the therapeutic and the selectivity, sensitivity, precision, and robustness of the assay.1 The FDA explicitly allows employment of a highly sensitive PD marker or properly designed PK assay, or both, that generate data capable of informing clinical activity, in lieu of a NAb assay. Nab assays, especially cell-based assays, can be highly variable and with low sensitivity, as they are often executed in cell culture media and measure particular functional endpoints.5 Therefore, hyper-variable cell-based NAb assays may not be as informative as a suitable PD or PK assay to indicate neutralizing antibody activities.
PRE-EXISTING ANTIBODIES
Frequently, humans may have antibodies to components of a therapeutic. For example, PEGylation is a common modification of certain proteins, which can reduce the immunogenicity of a protein, and prolong the circulatory life of a protein or improve water solubility of certain proteins. However, people can have pre-existing antibodies against it, given its frequent use in products, such as cosmetics. The fact that people entering clinical trials may already have pre-existing antibodies challenges the statistical analysis traditionally used to differentiate between positive and negative assay results.
The challenge of pre-existing antibodies is to determine the cut-point that adequately differentiates negative ADA, pre-existing antibodies, and true ADA-positive samples and subsequent data reporting. The 2019 guidance provides more details on how to manage the statistical calculations on cut-point during method validation as well as discussing reporting strategies for capturing data around pre-existing antibodies. It gives clear definition of treatment-boosted ADAs, which refers to the situation in which there are pre-existing antibodies and the titer of antibodies increases after exposure to the therapeutic protein product.
DOCUMENTATION REQUIREMENTS
Prior to the 2019 guidance, immunogenicity data were dispersed throughout the electronic common technical document (eCTD), the standard format for submitting to the FDA, presenting challenges for reviewers to understand the big picture of a potential therapeutic protein’s immunogenicity profile. The 2019 guidance provides detailed direction on documenting immunogenicity and requires an integrated immunogenicity summary report that gives a clear summary so FDA reviewers can understand the immunogenicity data up front. In addition, the FDA advises sponsors to arrange the integrated summary into distinct sections:1
-The Immunogenicity Risk Assessment should include “a concise immunogenicity risk assessment specific to the therapeutic protein product” as guided in FDA’s Immunogenicity Assessment for Therapeutic Protein Products guidance.
-The Tiered Bioanalytical Strategy and Assay Validation Summaries section should summarize immunogenicity assessment strategies used during each phase of a clinical program and provide links to method development and validation reports for pivotal clinical studies.
-For the Clinical Study Design and Detailed Immunogenicity Sampling Plans section, FDA guides sponsors to provide the immunogenicity sampling plan for all clinical studies where immunogenicity assessments were performed as well as sampling time points for immunogenicity and PK of the therapeutic protein.
-The Clinical Immunogenicity Data Analysis section should provide a summary of immunogenicity analyses for all clinical studies with an immunogenicity component as well as detailed discussion on the impact that pre-existing or treatment-boosted or treatment-induced antibodies have on PK, PD, efficacy, and safety of the therapeutic protein product.
-For the Conclusions and Risk Evaluation and Mitigation Strategies (REMS) section, FDA requests how the candidate therapeutic protein affects the safety and efficacy of the product for the subject population. It should also show how immunogenicity will be monitored post-marketing and how it will be incorporated into any REMS. Finally, FDA requests a discussion around life cycle management of approved immunogenicity assays.
CONCLUSION
The 2019 FDA guidance on immunogenicity assessment intends to have the industry adopt a risk-based approach to fully understand the potential immunogenicity of the therapeutic proteins they are studying, thus to mitigate the impact of unwanted immune responses. The 2019 guidance adds clarity in method development, validation, and reporting processes. This article provides an understanding of the evolving immunogenicity assessment and current considerations for anti-drug antibody assay development. It should be pointed out that immunogenicity should not be evaluated in isolation. The treatment emergent antibodies should be assessed in conjunction with the structure of the therapeutic proteins, patient characteristics, and disease involved; and the impact of immunogenicity should be evaluated with pharmacokinetics, pharmacodynamics, sustainable of clinical response, safety, and efficacy of the protein therapeutics. These factors are interlinked and contribute to patients’ immunogenicity profile. And because of these reasons, the FDA recommends providing an Integrated Summary Report of Immunogenicity in BLA submission that clearly defines the identification of risks, results for evaluation of all relevant risks and risk mitigation consideration.
SUMMARY
Immunogenicity assessment is one of the key elements in a biotherapeutic’s development process. Each novel therapeutic protein and its assay system can have its unique product-specific challenges. With scientific and regulatory expertise, a seasoned bioanalytical partner can help biopharma companies ensure that the bioanalysis and immunogenicity assessment for their developmental drug meet evolving regulatory requirements, provide resolutions to the challenges, and empower your success.
REFERENCES
- FDA, Guidance for Industry: Immunogenicity Testing of Therapeutic Protein Products – Developing and Validating Assays for Anti-Drug Antibody Detection (Silver Spring, MD, January 2019).
- FDA, Guidance for Industry: Immunogenicity Assessment for Therapeutic Protein Products (Silver Spring, MD, August 2014).
- Shen M, et al. Statistical evaluation of several methods for cut-point determination of immunogenicity screening assay. J Biopharm Stat. 2015;25(2):269-279.
- Mire-Sluis AR, et al. Recommendations for the design and optimization of immunoassays used in the detection of host antibodies against biotechnology products. J Immunol Methods. 2004;289(1-2):1-16.
- Wu B, et al. Strategies to determine assay format for the assessment of neutralizing antibody responses to biotherapeutics. AAPS J. 2016;18(6):1335-1350.
Leon Shi, PhD, Head of Biometrics, IMD, is the Biostatistician and head of Biometrics of IMD. His main duty includes preparing the Statistical Analysis Plan (SAP), reviewing trial protocol, creating summary tables/data listings/figures, sample size calculation, Standard Analysis, as well as, modeling and simulation. He holds a doctoral degree in Statistics from Oklahoma State University. He has accumulated over 15 years of experience in data analysis, SAS programming and mathematical modeling. During this period, he has participated in over 40+ Clinic trials with more than half of them including FDA Submission.

Lan Li is Vice President, Bioanalytical Services at WuXi AppTec Laboratory Testing Division. She has over 20 years of experience in the pharmaceutical industry in the United States, publishing numerous peer-reviewed articles in top scientific journals. Prior to joining WuXi AppTec, she worked for Alexion Pharmaceuticals, where she played critical roles in the discovery and development of Alexion’s drug products, holding positions of the Head of Bioanalytical Development and the Leader of Research Strategy, and contributed significantly in marketing approval and label expansion of the biotherapeutics.

Dr. Jing Shi is Executive Director and Global Head of large molecule Bioanalysis of WuXi AppTec Laboratory Testing Division with extensive experience in global biotech/pharma and CRO industry. She joined WuXi AppTec in 2014 and is the head of China Immunochemistry Bioanalytical department, managing multisite operations. Her team provides bioanalytical method development, validation and sample testing services under GLP/GCP. Dr. Shi previously held leadership positions with AstraZenica and Sigma in the United States. She has extensive working experience at various drug development stages including cell line development, process development, toxicology, biologics drug substance/drug product characterization and preclinical/clinical bioanalytical analysis. In her most recent role with Sigma, she was the head of the Immunoassay laboratory, responsible for GMP lot release/stability testing and GLP bioanalytical testing using immunochemistry- or cell-based platforms. Dr. Shi obtained her B.S. in Cell Biology and Genetics from Peking University and Ph.D. in Cell Biology from University of Virginia.
Total Page Views: 10332