Issue:September 2021
HOT MELT EXTRUSION - API Bioavailability: Suspending Hydrophobic Drugs in a Solid Solution
INTRODUCTION
As defined in the International Conference on Harmonization (ICH) Guidance for Industry, Q7A Good Manufacturing Practice Guidance for Active Pharmaceutical Ingredients (APIs), an API is any substance or mixture of substances intended to be used in the manufacture of a drug (medicinal) product.1 The API, when used in the production of a drug, becomes an active ingredient that is intended to furnish pharmacological activity or other direct effect in the diagnosis, cure, mitigation, treatment, or prevention of disease or to affect the structure and function of the body. While many APIs have therapeutic potential, that doesn’t mean they automatically function as effective drugs. Some APIs are innately hydrophobic, with poor bioavailability. Others are more hydrophilic, which results in higher bioavailability leading to a lower dose requirement to exhibit the intended pharmacological effect.
Of the new chemical entities currently in development, many present challenges for drug developers. More than 50% are excessively hydrophobic and fall into the Biopharmaceutical Classification System (BCS) Classes II, having high permeability, and IV, low permeability, through the gut wall, respectively.2 An additional ~25% fall into BCS Class III and are hydrophilic but display low permeability. It’s up to formulation scientists to determine how to incorporate these APIs into a drug formulation that is easily dissolved and absorbed in the body – preferably at the lowest effective concentration possible to minimize potential side effects. This is when hot melt extrusion (HME) comes into play. This technique enables the formulation of drugs into a solid dispersion, thereby increasing efficacy and safety of the drug product. HME can also be used to create time-release formulations that precisely control the concentration of a drug delivered to a patient over time.
While HME is a uniquely valuable tool for pharmaceutical developers, it requires specialized knowledge. As discussed further, not all APIs are compatible with HME and hence may not be a candidate for the method. For those that are, careful attention to the formulation quality attributes that include excipient selection, dosage form design, analytical testing, and stability are required to maximize the efficacy and quality of the final product.
BALANCING SOLUBILITY & STABILITY
Generally, APIs that are hydrophobic or that have a high molecular weight need to be “modified” for human metabolism, above and beyond the standard additives that are used for preservation, stability, and dosage form design. Furthermore, poorly soluble, lipophilic APIs are most stable in a crystalline state, which lessens bioavailability. Formulation scientists must overcome these conflicting requirements to create drug product formulations that can be easily absorbed by the body, while compensating for the reduction in stability associated with conversion of APIs from crystalline to an amorphous state. In some cases, the result is a compromise, where manufacturers create a formulation that allows an API to remain in a partially bioavailable state to preserve its stability. However, the per unit dose of API is usually increased to compensate for this reduction in bioavailability.
Although this technique delivers the necessary amount of API with required bioavailability to the body, it can produce a number of undesirable effects as the API concentrations rise. Drug product manufacturers may encounter safety concerns in production related to higher API concentration, increased risks of patient toxicity, and higher costs per unit dose. While challenging, HME can overcome each of these drawbacks.
HME APPLICATIONS
HME is a highly efficient continuous manufacturing process that uses high heat and shear forces to disperse a chemical in a mixture to form a solid dispersion. A solid dispersion created by HME is the distribution of one or more hydrophobic APIs into an inert hydrophilic carrier at solid state prepared by melting (fusion), which increases the surface area of the particles and in turn increases the dissolution rate, resulting in an increased bioavailability of a poorly soluble drug. However, because of the extreme conditions required for the HME manufacturing process, only relatively thermostable APIs are candidates for this approach. While any thermostable APIs can be formulated using HME, hydrophobic compounds that cannot be processed by other techniques are also prime candidates. This technique increases their bioavailability and dissolution rates, reducing the amount of API necessary for each dose, while other excipients can be leveraged to preserve their stability.
In addition to bioavailability, drug manufacturing with HME offers additional advantages, including the following:
- Masking the taste of bitter APIs in the final product
- Developing timed-release oral formulations or implantable devices
- Producing thin films (an increasingly popular and convenient method of oral drug delivery)
While HME addresses a key niche in pharmaceutical manufacturing, it is not a pharmaceutical invention. The technique originated in lead pipe manufacturing in the late 1800s. During the 1900s, manufacturing applications for HME took off in the rubber, plastic, and food industries in a wide variety of products. The common requirement is that all components of the mixture need to be evenly distributed at a molecular level. In the 1970s, pharmaceutical manufacturers adopted the HME technique for drug production, realizing its potential to generate chemical mixtures that overcame long-standing roadblocks in the field.3
SELECTING THE RIGHT EXCIPIENTS
Every API has unique chemical properties that facilitate its pharmacological effect. To ensure an API’s efficacy, each additional drug ingredient (excipient) must be carefully selected to complement these properties and its intended function.
Selecting the correct material and carrier composition of these functional excipients is critical to the HME manufacturing process. In fact, the precise combination directly affects the ease with which an API is converted into a molecular dispersion of sufficient purity. In the manufacturing process, excipients need to be carefully selected to minimize API degradation during the high heat and shear conditions, maximizing the stability and pharmacological performance of the final product.
As with a wonderful food recipe, every HME formulation has a base component (the food product) that is modified as needed by additional ingredients (such as the seasoning the food product is enhanced with: salt, pepper, garlic, onion, sugar, oil, butter, etc). The matrix carrier forms the base of the API drug formulation. As such, the most important quality of a matrix carrier its miscibility – it’s ability to dissolve an API in molten form and then, when solidified, release it into the surrounding environment at an appropriate rate. As an API can only be dissolved in a carrier’s molten state, the melting temperature and/or glass transition temperature of a carrier must be low enough that it minimizes temperature-induced degradation of the API and thereby the generation of impurities. Furthermore, due to temperature changes during the HME manufacturing process, matrix carriers must be capable of maintaining their integrity throughout the cycle of melting, mixing, and solidification. Finally, once cooled after manufacturing, a carrier must be stable and functional in its final dosage form. Common materials that meet these requirements tend to be low melting point waxes (eg, microcrystalline wax) or polymers (eg, ethyl cellulose, povidone polymers).
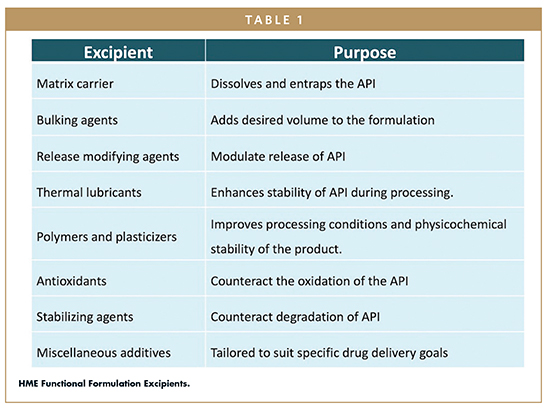
Other classes of functional excipients must also be carefully selected to support the API’s activity. These include bulking agents, release-modifying agents, polymers and plasticizers, antioxidants, and other stabilizing agents (Table 1).4,5 Developers should consider working with a manufacturing partner, such as Avomeen, for guidance on which chemicals in each class will form a pure molecular dispersion of the API. This in turn maximizes the drug’s performance and reduces its degradation during manufacturing, distribution, and storage.
THE PROCESS
To perform HME, all ingredients are fed through a feeder into an extruder consisting of a barrel and pipe (Figure 1). The temperature and shear forces within the barrel controlled in a fashion to convert all ingredients into a molten form. Subsequently, depending on manufacturing needs, one or more rotating screws push the mixture through the extruder. This process creates a uniform molecular dispersion, ultimately forcing the mixture through a die that gives it the correct size and shape. An added benefit is that the HME technique is very versatile – the product may also be flattened into a thin film or formed into a pellet or sphere.
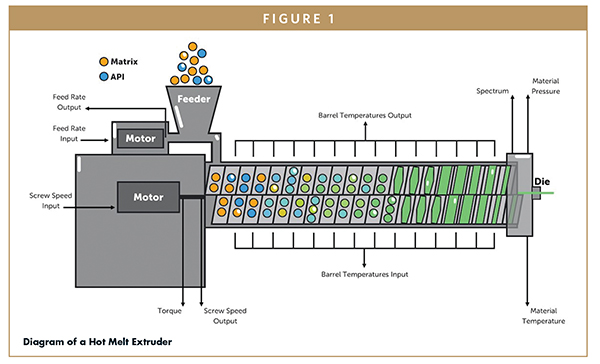
The ingredients of any formulation have a unique chemical makeup, and elements of the HME manufacturing process must be optimized to suit these chemical properties. At the basic level, the temperature at which the process occurs must be tailored to prevent the degradation of any of the formulation materials. Additional considerations include the screw design, pitch, and rate at which the screw pushes the mixture through the extruder and the fluidity of the mixture, both of which are important for creating conditions for a complete molecular dispersion.
Throughout a drug’s development and manufacturing, the quality of the product must be inherent to process (quality by design) and evaluated and controlled throughout the process and production train.6 For these purposes, Avomeen can offer partners in-process controls, process analytical technology, analytical capabilities like Raman and Near Infrared (NIR) spectroscopy, Differential Scanning Calorimetry (DSC) systems, and ultrasound to assess the quality of the final product.
WHY CHOOSE HOT MELT EXTRUSION?
Developing a formulation using HME can be a complicated process that requires the conditions, ingredients, and their concentrations to be optimally balanced to suspend the API into the polymer matrix. So why do some developers prefer this technique? There are several important factors: HME can be adapted for continuous manufacturing, it is modular, and it is an efficient method that produces highly efficacious drugs with lower concentrations of API per dose, making them safer for patients to take. Furthermore, HME is compatible with in-process controls and process analytical technology that enable developers to fine-tune their manufacturing processes in real time. Additionally, HME manufacturing is cost efficient and safer for workers because harmful solvents are not required to dissolve APIs, which are instead well-contained in closed systems as they are being prepared. This limits accidental drug exposure to employees and limits the amount of ingredients that escape into the environment during manufacturing. HME is also a fast process, with downstream steps seldom needed to reach a finished product. For this reason, there is some flexibility when it comes to an API’s stability in the face of high temperatures: while highly thermostable APIs are natural candidates for HME, APIs and excipients that are moderately thermostable, particularly those not suitable with other manufacturing techniques, may be considered. However, some APIs, such as antibiotics, proteins, and peptides, are categorically not thermostable and therefore cannot be formulated using HME.
In all, the rules dictating which APIs and excipients are suitable candidates for HME are highly nuanced. Only after the proper preformulation activities, design of experiments (DOE), and methodical characterization of a specific API’s stability can developers and their partners determine if a formulation will lend itself well to this technique. Although complicated, HME is worth considering because it introduces a wide range of formulation possibilities. The technique can incorporate numerous poorly soluble APIs into virtually any kind of solid, stable dosage form, including immediate, orally disintegrating, and controlled-release tablets, softgel capsules, thin films, microencapsulated drugs, nanoparticles, floating drug delivery systems, targeted drug delivery systems, intravaginal rings, stick packs, and intraocular or subcutaneous implants. No matter the dosage form, the HME manufacturing process enhances the bioavailability of poorly soluble APIs by incorporating the API into a hydrophilic matrix and/or pre-dissolving the API in a non-crystalline, amorphous state.
In an HME formulation, it is possible for a greater proportion of the API to reach the systemic circulatory system, requiring a lower concentration to produce the desired therapeutic effect. Formulations with smaller doses usually result in fewer off-target side effects and are therefore safer for patients to take. Moreover, for APIs that must be administered in relatively large amounts, a boost in bioavailability can significantly reduce the volume or number of doses a patient must take. HME formulation can also be remarkably effective at masking unpleasant tastes of APIs. For example, by adding an excipient that entraps the bitter tasting API into its matrix, thereby reducing the interaction of the API with the taste buds. Collectively, these benefits all promote drug compliance by improving the patient’s experience.
Complex dosing strategies may also be incorporated into drugs manufactured through HME. Specific polymer carriers, such as ethyl cellulose or carnauba wax, can be used to control an API’s diffusion rate so that a precise dose is released into the body continuously over days, months, or even years. Elaborate formulations can also be made using polymeric carriers of varying molecular weights combined with low molecular weight sugars, sugar alcohols, and waxes to produce drugs that carry reservoir systems capable of releasing varied amounts of one or more APIs at the same time. Overall, these controlled-release drugs ensure that a patient is receiving a uniform dose of the API while reducing the need for patients to manually control how much of a drug is in their system at a given time.
MANUFACTURING PARTNERS CAN HELP
To facilitate the process of HME formulation, developers can draw on the expertise of a manufacturing partner, such as Avomeen, that is well-versed in the HME technique from start to finish. Developers can save time and money by leveraging the experience of a suitable partner to efficiently select optimal excipients in the formulation that are best suited to a particular API, fine-tune the processing parameters, and develop analytical methods that satisfy regulatory guidelines.
At minimum, a partner’s experience in pharmaceutical formulation development should extend to novel drug delivery systems, including HME. A practice of utilizing the Quality by Design (QBD) approach to develop drug products for Investigational New Drug (IND) Applications and Abbreviated New Drug Applications (ANDAs) is also beneficial, as this tactic is meant to create products of the highest quality while minimizing future unexpected problems.3 Partners should also have knowledge of preformulation testing, including DOE, drug-excipient compatibility testing, wettability and solubility profiling, rheological studies, determination of flow properties, and physicochemical testing of early stage drug product prototypes, such as structural and stability characterization and impurity profiling. Finally, it is advantageous if a manufacturing partner can support the development and validation of analytical methods to test the quality attributes of a new formulation. These methods should be developed and comply with International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (ICH), Food and Drug Administration (FDA) and Current Good Manufacturing Practice (cGMP) guidelines. Important parameters include analytical guidelines for in-process control, release testing, and stability monitoring of pharmaceutical formulations. Together, a developer and a manufacturing partner with a strong understanding of the principles of HME can support successful HME-based drug development from start to finish.
REFERENCES
- International Conference on Harmonisation (ICH) Guidance for Industry, Q7A Good Manufacturing Practice Guidance for Active Pharmaceutical Ingredients (API), September 2016.
- Nikolakakis I, Partheniadis I. Self-Emulsifying Granules and Pellets: Composition and Formation Mechanisms for Instant or Controlled Release. Pharmaceutics. 2017;9(4):50. Published 2017 Nov 3. doi:10.3390/pharmaceutics9040050.
- Patil H, Tiwari RV, Repka MA. Hot-Melt Extrusion: from Theory to Application in Pharmaceutical Formulation. AAPS PharmSciTech. 2016;17(1):20-42. doi:10.1208/s12249-015-0360-7.
- Crowley MM, Zhang F, et al. (2007) Pharmaceutical Applications of Hot-Melt Extrusion: Part I. Drug Development and Industrial Pharmacy, 33:9, 909-926, DOI:10.1080/03639040701498759.
- Repka MA, Battu SK, et al. (2007) Pharmaceutical Applications of Hot-Melt Extrusion: Part II, Drug Development and Industrial Pharmacy, 33:10, 1043-1057, DOI: 10.1080/03639040701525627.
- Yu LX, Amidon G, Khan MA, et al. Understanding pharmaceutical quality by design. AAPS J. 2014;16(4):771-783. doi:10.1208/s12248-014-9598-3.
To view this issue and all back issues online, please visit www.drug-dev.com.

Ameya Deshpande is a Formulation Scientist at Avomeen, where he leverages his extensive experience in pharmaceutical formulation development and knowledge of novel drug delivery systems, including hot melt extrusion. He earned his MS in Industrial and Physical Pharmacy from the University of Toledo. He and Avomeen’s team of formulators routinely go above and beyond to deliver to clients.
Total Page Views: 5418










