Issue:April 2020
FORMULATION FORUM - Rational Design & Development of Lipid-Filled Hard Capsules
With ever increasing percentage of water-insoluble (BCS II/IV) or low permeable (BCS III/IV) new therapeutic entities among drug pipelines, lipid-based drug delivery systems, together with two other main drug delivery technologies, ie, nano and amorphous systems, have become an important tool for the formulation development of those compounds. Lipid-based drug delivery systems enhance the oral bioavailability of drugs via three main mechanisms: (1) increasing dissolution and solubility by pre-dissolving drugs in lipid carriers, (2) increasing drug permeability in the GI tract by inhibition of P-gp and other efflux transporters, and (3) bypassing the first-pass metabolism of the drug through the lymphatic absorption processes. In addition, lipid-based drug delivery systems have the potential to decrease the food-effect and to increase reproducibility of the pharmacokinetic profile of those orally administered drugs by reducing erratic absorption.
A lipid-based drug delivery system typically is composed of a lipid carrier, co-solvent, surfactants, and co-surfactant. Depending on the surfactant level, it can be classified into (1) microemulsion (thermodynamic stable lipid concentrate with high level of surfactant); and (2) nano-emulsion, which is a pre-formed nano-system as a result of high-energy inputs and is kinetic stable in the aqueous phase.
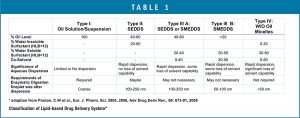
Lipid-based drug delivery systems can be also characterized into the following five categories (Table 1). The two most popular systems used for insoluble drugs are Type II/IIIA: Self-Emulsifying Drug Delivery Systems (SEDDS) and Type IIIB: Self-Microemulsifying Drug Delivery Systems (SMEDDS), forming microemulsions that are thermodynamically stable.
RATIONAL DESIGN & TECHNICAL FEASIBILITY
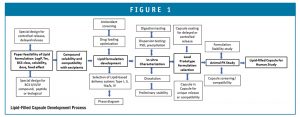
In order to ensure successful formulation development of lipid-based dosage forms, a thorough understanding of compound properties and a well-defined quality-by-design and development process (Figure 1) should be implemented.
Target Pharmaceutical Profiles
Compounds that will benefit most from lipid-based dosage forms are lipophilic, insoluble drugs that are poorly bioavailable through GI absorption (BCS II) and has a strong food effect. In some cases, the oral bioavailability of therapeutic entities, which are subject to efflux, high first-pass, low stability in GI fluids, or low permeability, such as peptides, biologicals, or BCS III/IV compounds, can be also improved by using lipid-based formulations. For drugs targeted to the intestine/colon, delayed release due to gastric irritation, or sustained release to achieve prolonged PK profile, utilizing solid/semisolid lipid materials or coating of capsules with insoluble or enteric polymer may be employed to achieve those goals. Typically, the ratio of therapeutic dose (mg) to the solubility (mg/mL) in the lipid carrier should be less than 0.5-5 mL to avoid pill burden; compounds with a low-medium dose requirement, log P>2, and a mid-low melting point will have a higher chance of success using the lipid formulation approach.
Solubility & Compatibility of Drug-Excipients
These lipidic excipients can be divided into the following categories: 1) oils such as long-chain triglycerides (LCTs), medium chain triglycerides (MCTs), mixture of mono-, di-, and tri-glycerides, and fatty acids; 2) water-insoluble surfactants: HLB < 12; 3) water-soluble surfactants: HLB ≥ 12; and 4) co-solvents. About 5 to 6 each of oils, surfactants, co-surfactant, and co-solvent (such as corn oil, soy bean oil, sesame oil, olive oil, castor oil, miglyol 812, captex 500, Solutol, labrasol, cremophor EL, poloxamer 188, Tween 20, Gelucire 44-14, TPGS, Tween 80; Phosal, Span 80, Span 20; Imwitor 988, Capryol 90, Lauroglycol 90, plurol oleic CC497, Labrafil M1944CS, Glycerin, Transcutol , PEG400, ethanol, propylene glycol) and their combinations can be selected and screened by drug solubility and compatibility. For compounds with poor permeability or efflux potential, the excipients that potentially can inhibit enzymatic efflux, increase tight junction permeability, or enhance lymphatic absorption can be added into the solubility screening study. Antioxidant(s) may be also introduced to protect the active drug from degradation due to incompatibility between drug and excipients.
Lipid Formulation Development & Characterization
The success of lipid-based formulations depends on the understanding of the compound’s physical-chemical and biopharmaceutical properties. For insoluble compounds with solubility- or dissolution-limited absorption processes, Type II-IV formulations could significantly improve its bioavailability by reducing the droplet size to the nano levels. For example, cyclosporine A lipid dosage form, Neoral®, is a Type III formulation that has a higher bioavailability than its Type II formulation (Sandimmune®). However, smaller droplet size does not always guarantee better in vivo performance. For example, Type I formulation of a lipophilic compound may promote lymphatic absorption and perform best in vivo, whereas a SMEDDS formulation may fail to improve its bioavailability due to precipitation of compound in the GI tract.
Based on an initial excipients screening study, a combination of excipients, solvents, and solubilizers can be used to enhance drug loading. Miscibility of excipients should be assessed using a physical stability study. In some cases, a DOE design can be utilized to screen antioxidant(s) and stabilizer(s) if the compound’s degradation in formulations is significant. The construction of phase diagrams is very valuable for optimizing self-emulsifying lipidic formulations (Type II-III A/B), defining the boundary of region where microemulsions forms.
Type I formulations consisting of single oil or oil mixtures require enzymatic digestion to be dispersed into oil droplet or micelles. Type II-III can be dispersed by itself in the aqueous medium into emulsion of different sizes with or without the help from enzymes due to utilization of surfactants. Type IV utilizes surfactants, and co-solvents without lipid oils can form micelles of <50 nm. However, due to potential risk of compound precipitation in the GI tract for Type II-IV formulations, an in vitro dispersion and in vitro dissolution in simulated GI fluids (FaSGF, FeSGF, FaSSIF, FeSSIF) should be employed during formulation screening and prior to animal studies.
Dosage Form Development
Based on the stability study and animal PK results, a lead prototype formulation can be selected for further development. To provide a dosage form that is commercially viable and convenient for human consumption, the lipid-based formulation can be filled into capsules and further packed into bottles or blisters. Due to manufacturing complexity and potential leaching of active compound into the shell, softgel capsules are normally not the first choice for encapsulation of lipid dosage forms at the early stage of clinical development. On the other hand, hard capsules, which offer flexibility for use from the early to commercial stages of development and different options for trade dress, are frequently chosen for lipid-based formulations. Studies should be conducted to select the type of capsule that is compatible with the formulation, can withstand the filling/banding process, and is stable throughout the shelf-life without causing leakage and brittleness of the capsule shells. In addition, the selected capsules should also be physically strong enough during the coating process, in case it will be coated with enteric polymers or sustained-release polymers to achieve delayed release into the lower GI tract.
A Case Example
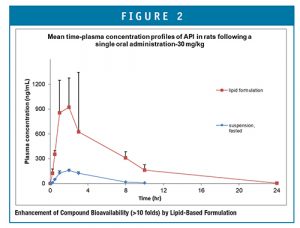
A compound was classified between BCS II (low solubility and high permeability) or BCS IV (low solubility and low permeability), which has a log P of ~3 and a meting point of ~120°C. Its aqueous solubility is extremely low, <1 μm/mL. The compound crystalline suspension had very low bioavailability in animal models that did not generate a dose-proportional exposure in the tox study. It was desirable to obtain a tox and human formulation that has an enhanced bioavailability. Based on the assessment of the compound properties, Ascendia’s Emulsol® Technology was utilized for lipidic formulation screening and in vitro assessment. Three lipid-based prototype formulations were developed and tested in animal models, resulting in a >10-fold increase in bioavailability (Figure 2). A hard gelatin capsule type that was compatible with the lead formulation throughout the filling, banding, drying, vacuum testing, and storage period was selected and used for cGMP manufacturing of clinical trial materials.
SUMMARY
Due to the benefits of lipid-based drug delivery in enhancing solubility/bioavailability and dosage manufacturing flexibility, lipid-filled capsules have gained popularity for use in clinical studies. Moreover, additional advantages in enhancing permeability, reducing food effects, and protecting therapeutic entities from degradation make the lipid-based dosage form attractive for delivery of small molecule compounds, peptides, RND/DNA, etc. Formulation development companies that specialize in poorly soluble molecules using GRAS material platforms, like Ascendia, can provide a decisive advantage in product formulation without increasing regulatory approval risk.

Jim Huang, PhD
Founder & CEO
Ascendia Pharmaceuticals
j.huang@ascendiapharma.com
www.ascendiapharma.com
Total Page Views: 6176