Issue:April 2013
EXCIPIENT UPDATE - A Real Eye-Opener: Advances in Hyaluronic Acid for Ophthalmology
The complexity of medical conditions related to the anatomy, function, and diseases of the eye can vary from eye dryness, which can be treated with lubricating eye drops, to pathological opacification of the eye, which requires cataract surgery and the use of viscoelastic devices during the removal of the natural lens of the eye Whether it is to enhance the hydration and lubrication of corneal surfaces, promote physiological wound healing, or extend the residence time of topically applied drugs in the eye, the benefits of incorporating hyaluronic acid (HA) in ophthalmic formulations are now well documented.1-3
Research into ophthalmic drug delivery has recently oriented itself toward sophisticated solutions, such as implantable devices. In addition t offering a better control of drug-release kinetics, these solutions give the possibility of more specific and targeted delivery. As the delicate structure of the eye requires pure and safe components preferably biodegradable and/or bioresorbable, HA provides a range of advantages owing to its exceptional water-binding, viscoelastic, and biological properties, offering many benefits for the development of novel ophthalmic solutions.
THE ROLE OF HA IN THE EYE
HA is a naturally occurring polysaccharide with distinct physicochemical properties that underlie its use as a viscoelastic tool and drug delivery solution in ophthalmolog applications. Within ophthalmology, HA was initially developed as an intraocular viscoelastic that was primarily used in cataract and other intraocular surgeries to protect the cornea post-procedure. Today, HA is widely used in many applications, including penetrating keratoplasty, trabeculectomy, retinal reattachment, and trauma surgery, as well as a treatment to relieve the symptoms of dry eye disease.
In the eye, HA is mainly found in the vitreous body, which is the transparent, colorless, gelatinous mass filling the space between the lens of the eye and the retin lining the back of the eye. HA’s function in the vitreous body essentially relates to providing shape, volume, and structure to an environment mostly composed of water (98% to 99%), as well as a small amount of solutes, such as salts, sugars, vitrosin, collagen, and other proteins. The use of HA in ophthalmic treatments is explained by its moisturization properties and its ability to extend drug-retention time and promote tissue healing. As a result, HA is a natural choice when evaluating possible excipients for drug formulations or ophthalmic devices.
REGULATORY CONCERNS FOR MANUFACTURERS
The popularity of animal-free ingredients is continuously growing, with regulatory authorities beginning to enforce tighter quality controls on products used i ophthalmic applications to improve safety and minimize risk to patients. Traditional commercial sources of HA are primarily derived from either rooster comb extraction or various attenuated strains of Streptococcus bacteria. However, these sources can potentially result in contamination risks from animal-derived proteins, viruses, or endotoxins. Moreover, both extracted HA and microbial-derived HA are purified using harsh organic solvents, which pose further health issues to patients.
In response to industry demand for safer sources of HA with a higher degree of purity, recent years have seen the emergence of biotechnological sources that eliminate the associated concerns and deliver increased safety and consistency, presenting new opportunities for ophthalmology applications both intraocular and topically.
BACILLUS-DERIVED HA(TM)
A Bacillus-derived fermentation process for the production of HA has been developed to overcome the manufacturing and safety challenges associated wit animal-derived sources. Bacillus subtilis is a non-pathogenic host whose products are Generally Recognized as Safe (GRAS) by the FDA. The process uses minimal medium, no animal-derived raw materials, and a water-based technique, which removes the use of organic solvents at any stage during the manufacturing process. The resulting HA is characterized by low amounts of nucleic acids, proteins, bacterial endotoxins, exotoxins, and microbial contamination, which reduces hypersensitivity reactions. Using biotechnology to produce HA not only increases safety, it allows for the manufacture of ophthalmic-grade HA polymers of various chain lengths and molecular weights. This, in turn, enables the production of ophthalmic solutions in varying viscosities.
The controlled Bacillus-derived production process affords a HA material with a wide-range of unique benefits. The findings of a recent study demonstrate the advantages of its use in ophthalmic formulation.
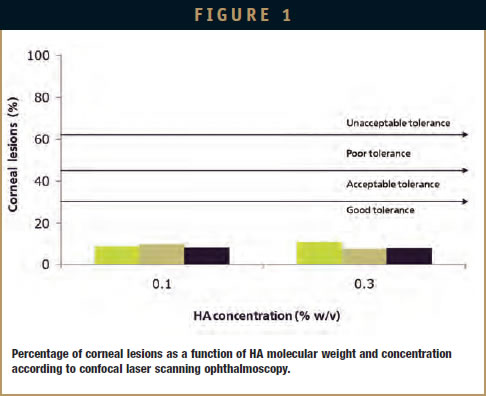
CORNEAL TOLERANCE OF HA
The corneal tolerance of HAs of different origins and molecular weights was evaluated by estimating the level of corneal lesions (epithelial cell loss), following repeated applications of three HAcontaining formulations onto the cornea (Figure 1). All HA samples, irrespective of their source, molecular weight, or concentration, induced a percentage of corneal lesions lower than 10%, which demonstrates good corneal tolerance. These findings also highlight the safety and biocompatibility of HA for ophthalmology applications.
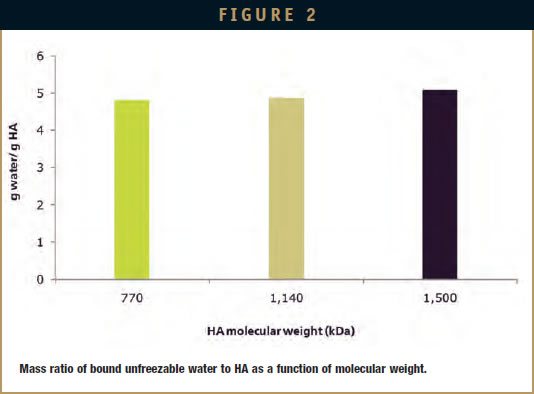
WATER-BINDING CAPACITY
The water-binding capacity of HAs from various sources and chain lengths was assessed by measuring the amount of HAbound unfreezable water using differential scanning calorimetry (Figure 2). Overall, HA’s water-binding capacity did not depend on molecular weight because the different HAs tested bound equally large amounts of water in the range 4 to 5 g/g HA. As a result of its water-retentive properties, Bacillus-derived HA has the potential to enhance moisturization of the ocular surface, while contributing to the stabilization of the precorneal tear film.
VISCOSITY
The performance of eye drops an artificial tears is related to their rheological properties and primarily depends on the nature, molecular weight, and concentration of the viscosifying agents employed. The non-Newtonian and shear-thinning properties of HA solutions make HA a viscosity enhancer of choice. Indeed, HA contributes to the uniform distribution of ophthalmic solutions on the surface of the eye while decreasing their drainage rate. This results in improved lubrication and function. However, highly viscous HAbased preparations can lead to increased blinking frequency, transient blurry vision, and ocular discomfort. Solutions incorporating Bacillus-derived HA possess well-defined rheological properties and feature optimal viscosity profiles for increased comfort and efficacy.
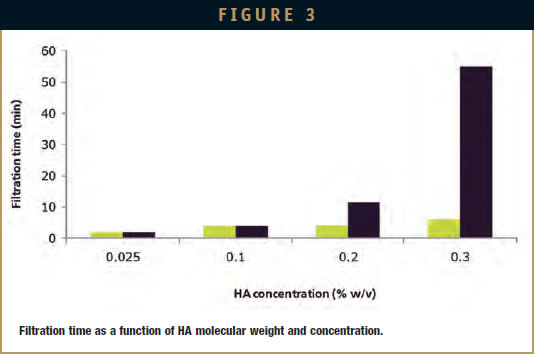
FILTRATION
The filtration times of a Bacillusderived HA solution and a solution derived from Streptococcus are presented in Figure 3. Up to a polymer concentration of 0.1 (w/v), HA molecular weight did not have an influence on the filtration time. However, at 0.2% and 0.3%, the filtration time of the higher-molecular-weight Streptococcus HA solution was three and seven times longer respectively than that of the Bacillus HA solution. At 0.3%, the Bacillus HA solution was filtered in less than 10 minutes against nearly 1 hour for the Streptococcus HA. The short filtration time of Bacillus-derived HA makes it easy to handle and helps reduce the manufacturing time of preparations sterilized by filtration.
HEAT STABILITY
Studies have shown that Bacillus HA remains stable during the heat sterilization of ophthalmic solutions. After treatment at 121°C for 16 minutes, Bacillus HA was shown to retain 82% of its initial molecular weight against 60% for a Streptococcusderived HA of the same starting chain length. This enhanced stability upon heating is most likely related to the purity of Bacillus HA. As a result, formulations containing this source of HA can be heatsterilized under standard conditions without compromising final product viscosity.
DRUG DELIVERY
As a result of its viscosity-enhancing properties, HA can be used as an efficient carrier for ophthalmic therapeutics. In this respect, Bacillus HA presents goo compatibility with a variety of drugs such as ciprofloxacin, diclofenac, and dexamethasone. Increased lacrimation and tear turnover following the application of ocular formulations most often lead to short precorneal residence time and, as a result, poor drug bioavailability. According to gamma scintigraphy, the precorneal residence time of Bacillus-derived HA is similar to that of Streptococcus-derived HA of higher molecular weight at the same concentration. Furthermore, the incorporation of HA in drug-containing ophthalmic solutions can increase drug retention in the tear fluid, along with drug contact time with the ocular surface, consequently improving drug bioavailability. The underlying mechanisms for drug retention are believed to be largely related to viscosity, bioadhesion (mucoadhesion), and physical attachment.
The Bacillus-derived fermentation process offers a source of HA with a reproducible molecular weight and narrow size distribution. In addition, the HA offers improved processability due to the porosity and reduced size of it spray-dried particles and can dissolve much faster than HAs manufactured with an organic solvent-based process. This reduces processing time at large scale while contributing significant savings on manufacturing costs. A high degree of purity of the material also permits sterilization by autoclaving without significant loss of product properties.
SUMMARY
The use of HA in ophthalmic treatments is continuously growing due to its ability to extend drug-retention time and promote effective tissue healing. Bacillusderived HA offers new opportunities for ophthalmic applications by providing a safe and biocompatible source that can streamline manufacturing processes, while offering convenient application and increased patient comfort and compliance. The latest technology ensures high levels of safety, consistency, and stability, conferring numerous benefits to both manufacturers and patients.
REFERENCES
- Nakamura M, et al. Characterization of water retentive properties of hyaluronan. Cornea. 1993;12:433-436.
2. Tani E, et al. Effects of various eye drops on corneal wound healing after superficial keratectomy in rabbits. Japan J Ophthalmol. 2002;46:488-495.
3. Saettone MF, et al. Mucoadhesive ophthalmic vehicles: evaluation of polymeric low-viscosity formulations. J Ocul Pharmacol. 1994:10:83-92.

Hans Ole Klingenberg is Director for the Global Marketing group in Novozymes Biopharma. Hans Ole has been with the company for more than 10 years and has held various positions in the area of corporate business development, with a focus on establishing new business entities for Novozymes in the biopharmaceutical industry. Since 2007, he has been working in Novozymes’ Biopharma business with a focus on marketing, and is commercially responsible for the establishment of the company’s Hyaluronic Acid business franchise. Mr. Klingenberg is a graduate of Copenhagen University with a Bachelor’s in Chemistry and Master’s in Economics. He is based in Denmark.
Total Page Views: 4575