Issue:May 2024
DRUG & DEVICE DEVELOPMENT - Integration of siRNA, Nanoparticles & Capsule Endoscopy for Treatment of Inflammatory Bowel Disease
INFLAMMATORY BOWEL DISEASE
Inflammatory Bowel Disease (IBD) is a chronic condition of the gastrointestinal tract that affects approximately 3.1 million adults in the US, representing 1.3% of the adult population.1 There is currently no cure for this disease, and treatment options prioritize the management of symptoms. Typical manifestations of IBD include diarrhea, abdominal discomfort, rectal bleeding, and reduced body weight. The range and severity of these symptoms can vary, and patients often experience periods of remission and active disease flares.2 IBD can be further divided into two subcategories: ulcerative colitis and Crohn’s disease, which are both characterized by abnormal immunological responses in the gastrointestinal (GI) tract and the bacterial microbiome. Ulcerative colitis (UC) affects a continuous region of the colon and rectum, which experiences inflammation and excessive ulcers on the outermost mucosal layer of the GI tract. Crohn’s Disease involves inflammation and ulcers across all regions and layers of the gastrointestinal tract, with affected regions presenting in patches.
While many established treatments exist to manage symptoms, each has its disadvantages. Aminosalicylates have limited efficacy in severe cases and can cause gastrointestinal discomfort. Corticosteroids are efficacious at providing short-term relief but are not recommended for prolonged use due to side effects, which include osteoporosis, myopathy, diabetes, and hypertension. Immunomodulators lower inflammation through immune response suppression, which increases infection susceptibility and liver toxicity. While biologics are more potent and targeted in their inhibition of inflammation, they increase the risk of infections, are high in cost, and have lowered patient compliance due to the route of administration.2 Overall, current IBD therapeutics are reactionary because they work to inhibit or modulate active inflammatory responses. Therefore, there is a necessity for preventative treatments that offer a high degree of specificity and target the root cause of inflammation.
CAPSULE ENDOSCOPY
IBD is most commonly diagnosed via endoscopic procedures, such as a colonoscopy. Though they are effective, colonoscopies are expensive and inconvenient, requiring patients to empty their bowels, follow strict liquid diets for 24 hours, and undergo temporary sedation during the procedure.3 They are also limited to imaging within the colon due to length, size, and flexibility restrictions of the endoscope instrument. As an alternative, researchers have developed capsule endoscopy systems, which involves an ingestible pill with an embedded camera that can take images of the entire GI tract, including the esophagus and stomach, at a lower cost and without requiring a complex procedure.4
Capsule endoscopy devices are currently used for the detection and diagnosis of IBD and have laid the groundwork for a novel area of research in the treatment of gastrointestinal diseases. Many medical device companies, such as Olympus, Jinshan, and Biocam, have introduced capsule endoscopes to the market. The PillCam™, developed by Medtronic, is the most well-known, and features a pill-shaped design enclosing a wireless camera. The PillCam SB model, once ingested, takes high-resolution images over a period of 8-12 hours and transmits its data wirelessly.5 More recently, Medtronic developed the PillCam COLON2™, which captures panoramic images of the gut and uses artificial intelligence (AI) to dictate image-capturing frequency.6
The accessibility, image-capturing capabilities, ingestible size, and AI technologies of PillCam devices are compelling reasons to continue studying capsule endoscopy for IBD treatment. However, despite the diagnostic abilities of the current PillCam devices, they are not commonly used after initial disease identification, and very few are under development specifically for drug delivery applications.
NANOPARTICLE-MEDIATED SIRNA DELIVERY FOR IBD
Small interfering RNA (siRNA) treats IBD by targeting and silencing specific genes involved in inflammatory and immune responses. siRNA molecules selectively down-regulate genes associated with diseases by cleaving mRNA sequences. For IBD, siRNA knocks down genes that code for inflammatory mediators, such as TNF-α, integrins, and inflammatory interleukins. This targeted gene silencing directly addresses the root causes of inflammation in IBD, offering a precise method to mitigate the disease’s effects. However, there are several barriers to targeted siRNA delivery. The negative charge, hydrophilicity, and large molecular weight of siRNA hinder its cell membrane penetration. Furthermore, while oral administration is often preferable due to increased patient compliance and ease of administration, it exposes siRNA to the GI tract’s acidic conditions and digestive enzymes.7
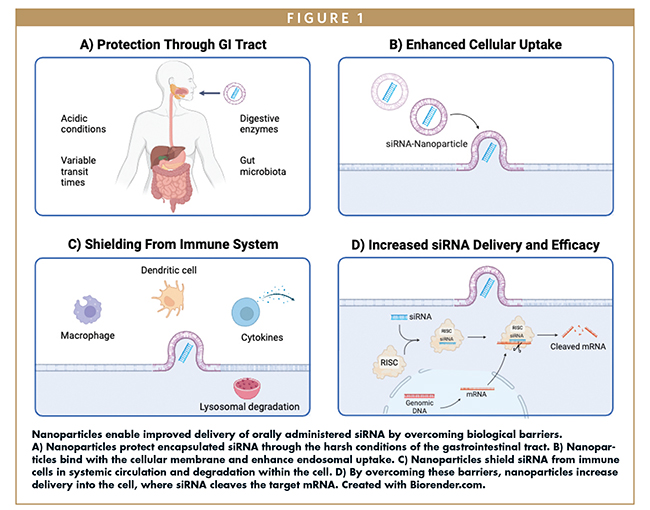
Nanoparticles have emerged as a promising solution for siRNA delivery. Nanoparticles are materials on the nanoscale that can be engineered to overcome biological barriers, including the harsh conditions of the GI tract, cellular binding and uptake, and the immune response in circulation and within the cell, and enable targeted delivery (Figure 1). The most common are administered orally and deliver siRNA that targets TNF-α, CD98, and Map4k4. Several nanoparticle carriers have shown efficacy in preclinical studies, including liposomes with hyaluronan and Dipalmitoyl Phosphatidylethanolamine (DPPE), polyethyleneimine-derived nanoparticles, calcium phosphate and Poly lactic-co-glycolic acid (PLGA) nanoparticles, chitosan-derived nanoparticles, and poly(amino acid) nanoparticles.8
Despite the potential of nanoparticle-mediated siRNA delivery to down-regulate inflammatory genes, it cannot precisely distinguish between diseased and healthy regions of the gut. Thus, targeted delivery to highly inflamed regions of the GI tract is difficult, and off-target effects may occur. Achieving precise delivery is challenging and is compounded by the lack of detection tools used in conjunction with treatment. Overcoming these hurdles is crucial for the successful use of siRNA therapies for the treatment of IBD.
INTEGRATION OF SIRNA DELIVERY & CAPSULE ENDOSCOPY
Capsule endoscopes and siRNA nanoparticle therapies have widely different application purposes for the diagnosis and treatment of IBD patients. Capsule endoscopy records real-time imaging data of the gastrointestinal tract, and the siRNA-nanoparticle therapies treat the root cause of inflammation in IBD. However, both have drawbacks that limit their individual utility. Currently, most capsule endoscopes with real-time imaging are not used after initial diagnosis as they are not engineered for therapeutic delivery. siRNA-nanoparticle therapies cannot precisely distinguish and target damaged regions and cells, resulting in off-target effects, material wastage, heightened immune responses, and tissue damage when used for prolonged periods. An integrated siRNA and capsule endoscopy system can address the pitfalls of each stand-alone technology and provide patients with a more effective therapy option. In this integrated system, the capsule endoscope will send imaging data to external software that triggers siRNA nanoparticle release based on the detection of swelling, ulceration, and strictures (Figure 2).
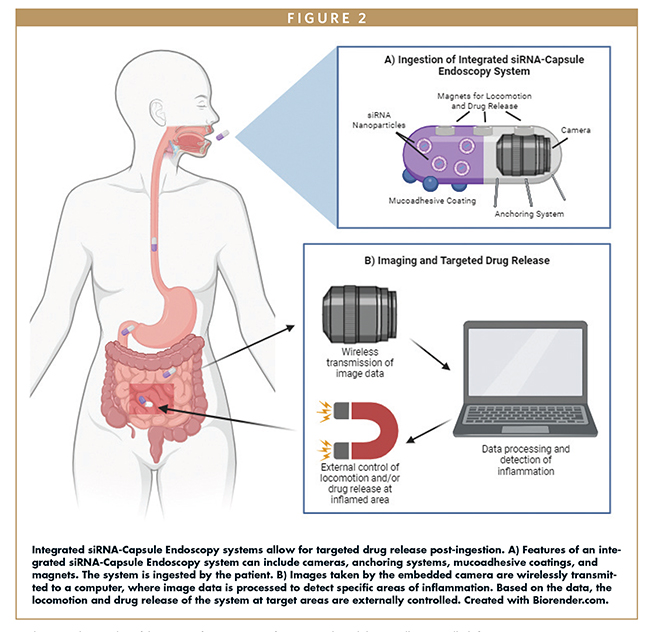
Due to the variable environment of the GI tract, several factors must be considered to develop an effective integrated capsule endoscopy drug delivery system. For example, the diameter of the GI tract and the presence of fluid vary significantly by patient. Therefore, integrated systems should fit within certain size constraints, include highly controlled drug-release mechanisms, and feature anchoring systems to attach to specific regions within the GI tract.9
The drug-release mechanism of a capsule endoscope needs to be strictly controlled to ensure that a precise drug dose is delivered at specific sites. In recent years, many different smart pill and capsule endoscope manufacturers have experimented with different active and passive release mechanisms of drugs for delivery to the GI tract. Three important examples are the RaniPill™, InteliSite®, and Enterion™ capsules. RaniPill uses a passive release mechanism in which the drug is encapsulated by a hydroxypropyl methylcellulose capsule in an enteric coating. This coating does not dissolve in low pH values found in gastric acid but dissolves and inflates a balloon when in the higher pH region found in the intestines. The balloon then exposes a biodegradable needle for direct deposition of the drug into the gastrointestinal wall. InteliSite contains a liquid drug in a 0.3-mL reservoir that is sealed with a thin layer of lubricant. The drug is released through a pre-programmed code on an external computer that provides activation energy. The system then uses a screw-pump release that delivers the drug in a passive, slow manner. Finally, the Enterion uses a radio-frequency transmitter to trigger a spring mechanism using magnetic impulses. The drug reservoir holds 1 mL of the drug and when triggered by an internal heating element, a piston rapidly releases the drug.10
Drug-release mechanisms for capsule endoscopes are still an active area of research. Uniquely, Lee et. al have developed a capsule endoscopy system that relies on magnets for locomotion and drug release, though it is not currently available on the market. Specifically, they created a system that captures images of the GI tract and actively delivers biodegradable therapeutic patches to target lesions via a robot-assisted magnetic actuator. The actuator controls a lid, capable of opening and closing to deliver multiple doses whenever an inflamed region is detected. Furthermore, embedded neodymium magnets allow the device to be precisely controlled with an external magnetic field, improving the accuracy of drug delivery.11
Traditionally, capsule endoscopy relies on the natural peristalsis of the GI tract for movement. To target specific areas of interest, anchoring systems that can resist peristalsis are required. Tethered legs or hooks are common anchoring systems that function by attaching to the intestinal wall while images are captured. Similarly, mucoadhesive patches or coatings can stick to the intestinal wall, and often biodegrade after use. Moreover, motors and actuators are frequently used for precise navigation and anchoring. Mechanical actuators often use tethered legs, rolling treads, and propellers for locomotion. The main limitation of mechanical actuators are their large size, which is primarily due to bulky mechanical locomotion devices and a need for energy storage. Magnetic actuation involves embedding a magnet in the capsule and orienting it through a magnetic field gradient external to the patient. Magnetic actuation emerged as a human-controlled mechanism but is now commonly completely computer-controlled.12
Many different release and anchoring mechanisms for smart capsule drug delivery in the GI tract are actively being researched today. By providing targeted and preventitive treatment, the combination of smart capsule endoscopy and siRNA delivery will change the landscape of IBD treatment.
FUTURE OUTLOOK
As new technologies emerge, an integrated capsule endoscopy and siRNA delivery system can be engineered with increasingly effective imaging systems, release mechanisms, locomotion machinery, dosing regimens, and anchoring systems. For example, artificial intelligence and machine learning are rapidly gaining traction in pharmaceutical and medical applications. They can play crucial roles in the identification of inflammation and the successful delivery of siRNA to that inflamed region. Another promising area for future work is the attachment of IBD-specific biomarkers to the capsule surface for chemical recognition and release of siRNA nanoparticles. Furthermore, the imaging capabilities of existing capsule designs can be improved with the use of blue and green light, which can increase the visibility of inflammation.13 Many other innovations are in development for nanoparticle-mediated siRNA delivery and capsule endoscopy, and the application of such technologies in an integrated system is key.
This article highlights a promising technology that can change the way Inflammatory Bowel Disease is treated. Current imaging technology can successfully identify inflammation, and current treatments can address active inflammation and manage symptoms. There remains a need for technology that can address the reactive nature and systemic effects of current treatments. The combination of siRNA nanoparticles, which target the root cause of inflammation, and capsule endoscopy, which enables targeted delivery, will be a significant step forward for patient care.
ACKNOWLEDGMENTS
The authors would like to express their gratitude to Dr. Nicholas A. Peppas, whose expertise and guidance have been invaluable throughout the research process. This paper would not have been possible without his support.
REFERENCES
- Xu, F.; Dahlhamer, J. M.; Zammitti, E. P.; Wheaton, A. G.; Croft, J. B. Health-Risk Behaviors and Chronic Conditions Among Adults with Inflammatory Bowel Disease — United States, 2015 and 2016. Morb. Mortal. Wkly. Rep. 2018, 67 (6), 190–195. https://doi.org/10.15585/mmwr.mm6706a4.
- Cai, Z.; Wang, S.; Li, J. Treatment of Inflammatory Bowel Disease: A Comprehensive Review. Front. Med. 2021, 8.
- Diagnosing Inflammatory Bowel Disease. https://nyulangone.org/conditions/inflammatory-bowel-disease/diagnosis (accessed 2023-11-27).
- Iddan, G.; Meron, G.; Glukhovsky, A.; Swain, P. Wireless Capsule Endoscopy. Nature 2000, 405 (6785), 417–417. https://doi.org/10.1038/35013140.
- Validation of SmartPill® wireless motility capsule for gastrointestinal transit time: Intra-subject variability, software accuracy and comparison with video capsule endoscopy – Diaz Tartera – 2017 – Neurogastroenterology & Motility – Wiley Online Library. https://onlinelibrary.wiley.com/doi/abs/10.1111/nmo.13107?casa_token=0qYEM6K2xloAAAAA%3APog03mHb3pivCj7Bd267mG7mg4z1A3YE0CZ4BqGhaue_gLMH-8HVkGyeiAsJcxiJX1BW5GVuvpkuSfYI (accessed 2024-03-30).
- PillCam COLON capsule endoscopy: recent advances and new insights – Samuel N. Adler, Yoav C. Metzger, 2011. https://journals.sagepub.com/doi/10.1177/1756283X11401645 (accessed 2024-03-30).
- Tokatlian, T.; Segura, T. siRNA Applications in Nanomedicine. WIREs Nanomedicine Nanobiotechnology 2010, 2 (3), 305–315. https://doi.org/10.1002/wnan.81.
- Mitchell, M. J.; Billingsley, M. M.; Haley, R. M.; Wechsler, M. E.; Peppas, N. A.; Langer, R. Engineering Precision Nanoparticles for Drug Delivery. Nat. Rev. Drug Discov. 2021, 20 (2), 101–124. https://doi.org/10.1038/s41573-020-0090-8.
- Scott, R.; Enns, R. Advances in Capsule Endoscopy. Gastroenterol. Hepatol. 2015, 11 (9), 612–617.
- Cortegoso Valdivia, P.; Robertson, A. R.; De Boer, N. K. H.; Marlicz, W.; Koulaouzidis, A. An Overview of Robotic Capsules for Drug Delivery to the Gastrointestinal Tract. J. Clin. Med. 2021, 10 (24), 5791. https://doi.org/10.3390/jcm10245791.
- Active Capsule System for Multiple Therapeutic Patch Delivery: Preclinical Evaluation | IEEE Conference Publication | IEEE Xplore. https://ieeexplore-ieee-org.ezproxy.lib.utexas.edu/abstract/document/10341491 (accessed 2024-03-20).
- Slawinski, P. R.; Obstein, K. L.; Valdastri, P. Capsule Endoscopy of the Future: What’s on the Horizon? World J. Gastroenterol. 2015, 21 (37), 10528–10541. https://doi.org/10.3748/wjg.v21.i37.10528.
- Muto, M.; Horimatsu, T.; Ezoe, Y.; Hori, K.; Yukawa, Y.; Morita, S.; Miyamoto, S.; Chiba, T. Narrow-Band Imaging of the Gastrointestinal Tract. J. Gastroenterol. 2009, 44 (1), 13–25. https://doi.org/10.1007/s00535-008-2291-5.

Nila Murali is a Chemical and Biomolecular Engineer from The Georgia Institute of Technology, where she collaborated on research with Dr. Anant Paravastu on the synthesis and modeling of Alzheimer’s beta-amyloid self-assemblies. She has previously worked at Somerset Therapeutics, Regeneron Pharmaceuticals, and Bristol Myers Squibb as a Process Development Engineer. Currently, she is working toward her PhD in Molecular Pharmaceutics and Drug Delivery at The University of Texas at Austin, focusing on inhalation drug delivery for chronic lung infection caused by Pseudomonas Aeruginosa.

Ravali Bhavaraju is a Biomedical Engineer from The University of Texas at Austin. She has worked in numerous aspects of drug delivery and has done extensive research with Prof. Nicholas A. Peppas in the biomedical engineering and pharmaceutical departments of The University of Texas at Austin. She has previously worked for Eli Lilly and Company and Stryker. Her research focus is on physiologically based pharmacokinetic modeling and drug delivery of siRNA for Inflammatory Bowel Disease.

Leia Jiang is a Biomedical Engineer from The University of Texas at Austin. She is continuing her studies with a PhD in Biomedical Engineering at Carnegie Mellon University, focusing on Tissue Engineering and Regenerative Medicine. She collaborated with Dr. Miguel Flores-Bellver at the University of Colorado School of Medicine on extracellular vesicles for therapeutic delivery in the eye. She also worked with Dr. Tyrone Porter at The University of Texas at Austin, on in vitro modeling of the blood-brain barrier.
Total Page Views: 4404