Issue:October 2023
DELIVERY TECHNOLOGY - Topical NeuroDirect™ Ketamine in the Treatment of Neuropathic Pain Syndromes: Fibromyalgia, Neuropathy, Radiculopathy & Causalgia/Complex Regional Pain Syndrome
NEUROPATHIC PAIN INTRODUCTION
Pain can be classified as nociceptive and transient; or, neuropathic and chronic.1 Nociceptive pain alerts of acute injury; and generally resolves after injury heals. Neuropathic pain, on the other hand, serves no physiologic purpose. It is the result of aberrant pain impulses relaying to central nervous system (CNS) from prior peripheral injury. It is chronic, unrelenting, and affects function and mood. Described in such terms as “burning, aching, electric-like, and constant,” it involves several different areas of CNS. (Figure 1).
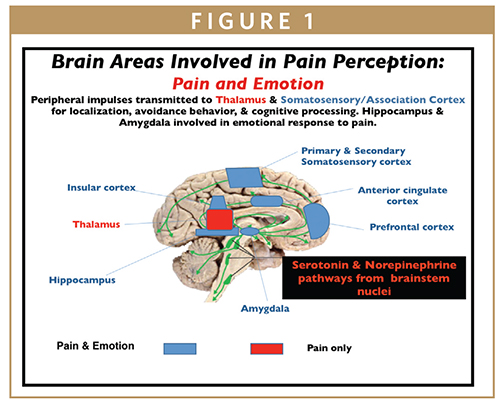
Figure 1 illustrates different areas of CNS affected in chronic neuropathic pain. Primary and secondary somatosensory cortices are involved, as well as areas subserving emotion, memory, and reward behavior. Neuropathic pain affects both physical and psychological aspects of human function.
With causalgia or complex regional pain syndrome, CRPS, up-regulated CNS structures cause spread of pain and vasomotor symptoms to parts other than the primary site of injury.
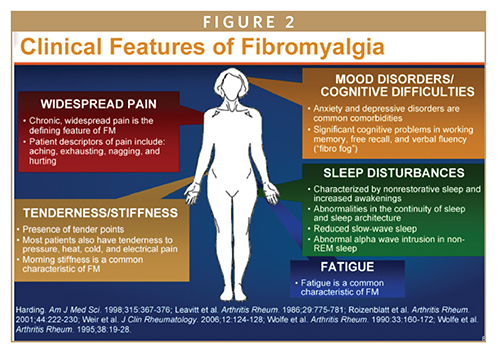
In fibromyalgia, the causative factor may be a remote traumatic event, separated in time, sometimes years, from events which later contribute to “total body pain,” the hallmark of the disorder. The initial event may be tied to emotional or physical abuse, or both; which remains embedded and unresolved in an individual’s psycho-social being. Later, an injury, seemingly trivial, causes the “dam to break” with body-wide symptoms of pain, stiffness, and weakness. Other symptoms that frequently accompany are depression, anxiety, mood swings, sleep loss, and chronic fatigue.2,3
Pain serves to alert of injury; left neglected, brain structures involved with pain perception up-regulate, resulting in heightened perception and other associated symptoms. Emotional pain increases such up-regulation more than physical pain. Both are influenced by norepinephrine, NE, and serotonin, 5-HT. In a heightened emotional state, physical pain is more acutely perceived; alternatively severe physical pain affects mood.
KETAMINE & THE NMDA RECEPTOR IN NEUROPATHIC PAIN
There has been much attention on the N-methyl-D-aspartate, NMDA, receptor antagonist, ketamine, for use in PTSD and neuropathic pain. Authors of this article published findings with NeuroDirectTM topical ketamine in treating PTSD and intractable depression in March 2023.4 Ketamine is thought to produce strong analgesia in neuropathic pain states through inhibition of the NMDA receptor.5,6
The NMDA receptor has excitatory glutamic function at spinal and supra-spinal sites involved in afferent transmission of nociceptive signals. In chronic pain states, prolonged nociceptive stimulation causes activation and up-regulation of NMDA receptors at dorsal horn synapses, resulting in increased and heightened pain signals to brain, so called “central sensitization.” This is the major contributing factor in producing a chronic neuropathic pain state.
There is increasing evidence NMDA receptor antagonists, such as ketamine, attenuate excessive nociceptive input to brain, thereby providing an alternative means to treating chronic pain syndromes.4 Other aspects of ketamine that may contribute to its analgesic effects include enhancement of descending inhibition and its anti-inflammatory effects.7-9
Antagonism of NMDA receptor by ketamine is thought responsible for its anesthetic and analgesic, as well as anti-depressive effects; the former, through prevention of “central sensitization.” The antidepressant action involves norepinephrine, serotonin, and dopamine.
NMDA receptors exist on peripheral nerves and skin-free nerve-endings, allowing receptor antagonism to occur at these sites with topically applied drugs. Accordingly, ketamine applied to skin at specific anatomical areas can provide pain relief and also alleviate depression and anxiety.10,11 Topically applied at the back of the neck at the hairline (BONATH), ketamine was found effective in treating PTSD and intractable depression.4
Persistent peripheral activation of NMDA receptors to spinal cord inter-neurons results in increased sensitivity to neural input, causing “central sensitization.”12-15 On the other hand, “peripheral sensitization” is acquired excitability of sensory nerves with decreased threshold to nociceptor activation.16
Accordingly, with location of NMDA receptors on both afferent somatic and visceral nerve axons, there is potential for treating various different pain conditions with ketamine.17
KETAMINE
Initially used as a general anesthetic, ketamine induces “dissociative anesthesia,” a trance-like state providing pain relief, sedation, and amnesia. Short-term IV infusions of ketamine produce potent analgesia only during administration. Prolonged infusions (4-14 days) provide more long-term analgesic effects, up to months. Side effects of ketamine include psychedelic symptoms (hallucinations, memory defects, panic attacks), nausea/vomiting, somnolence, cardiovascular stimulation; and, hepatotoxicity.18
In controlled settings, ketamine is fairly well tolerated. Regardless, close monitoring of patients receiving systemic ketamine is mandatory; with particular attention to CNS and hemodynamic effects. Pending additional definitive proof, ketamine administration should be restricted to patients with intractable depression and therapy-resistant severe neuropathic pain.
Despite IV ketamine not formally approved for neuropathic pain or PTSD, ketamine infusion clinics have popped up at major cities throughout the United States. Without insurance coverage of infusions, therapy can be cost prohibitive, from $300-$2,000 per IV infusion, depending on dose and indication for treatment. Infusions last an hour or more, followed by an observation period for vital signs and side effects. Psychiatric side effects are frequent as well as elevated blood pressure and nausea.
Even at low sub-anesthetic intravenous doses, psychiatric side effects are prominent. A majority of patients report feeling “strange, spacey, woozy, or floating” or having visual distortions or numbness. Also frequently mentioned are speech difficulty, confusion, euphoria, drowsiness, and concentration problems. Psychotic symptoms such as “going into a hole, disappearing, feeling melting, experiencing colors, and hallucinations” are described by some 10% of people. Dizziness, blurred vision, dry mouth, hypertension, nausea, body temperature changes, or feeling flushed are common non- psychiatric side effects. Accordingly, a several-hour period of observation is recommended following IV ketamine infusion. Patients are not recommended to drive home afterward.
Ketamine has not been approved in the US for PTSD or depression or for use in neuropathic pain. However, an enantiomer of ketamine (esketamine, Spravato®) has been approved as a nasal spray for treatment-resistant depression in the United States and elsewhere. It is not, however, approved for treating neuropathic pain. Furthermore, there is an associated Risk Mitigation and Management Strategy (REMS) with its use, and the drug is made available only at designated treatment centers. The restricted program called SPRAVATO REMS exists because of the risks of serious adverse outcomes from sedation, dissociation, and abuse and misuse. It may only be dispensed and administered in certified healthcare settings by a healthcare provider, with monitoring for at least 2 hours following administration.19
UNIQUE NATURE OF TOPICAL NEURODIRECT™ KETAMINE
It is apparent ketamine can play an important role in treating intractable symptoms of neuropathic pain and PTSD. But limiting use is expense, inconvenience, potential side effects, and impracticality as maintenance therapy. We reported previously on the efficacy and convenience of at-home treatment NeuroDirect topical ketamine cream in alleviating persistent symptoms of PTSD and intractable depression.4 We now report its efficacy in treating a wide variety of neuropathic pain conditions.
NeuroDirect (also known as Direct Effects™ technology) is a novel, patented delivery of neuro-affective compounds as cream applied to skin at the back of neck at the hairline, “BONATH.” BONATH is a critical area of anatomy where access to afferent neural input to spinal cord and brain is achieved cutaneously through Trigeminal and Vagal Nerve Complexes at the upper cervical nerve roots, C1-C4. Free nerve-endings under skin surface are activated by topically applied active drug, with neuro-chemical reactions occurring at specific receptors. Action potentials to the CNS as result of these chemical reactions provide therapeutic benefit. This occurs without requirement of drug entry into bloodstream, main source of side effects and drug interactions. Further, there are no restrictions placed by the blood-brain-barrier. The psychogenic effects encountered with intravenous, nasal spray, and other systemic ketamine uses are avoided. With NeuroDirect technology, benefits of psychedelic compounds may be achieved without concern for their potential systemic effects.5
Other neuro-affective compounds successfully used with NeuroDirect technology include: triptans, dopamine agonist apomorphine, tizanidine, phentermine, 4-amino pyridine; cannabinoids, in particular, CBD, CBG, and beta-caryophyllene; as well as opioids, amantadine, tramadol, and others. In these topical drug applications, therapeutic benefit was achieved within 10 minutes of application, as nerve impulses from skin free nerve-endings to brain travel at the same rate for all individuals. Without involvement of the bloodstream, usual systemic side effects associated with these compounds were not observed.
In summary, through mechanisms at NMDA receptors, various chemical and neuro-electrical processes responsible for symptoms related to neuropathic pain and PTSD may be addressed using a single compound, ketamine. Additionally, using ketamine with NeuroDirect technology allows potential undesirable side effects to be avoided, with therapeutic benefits achieved rapidly.
It is interesting to note both neuropathic pain syndromes and PTSD are abnormalities in brain pain processing with heightened perception and involvement of other physical and psychological functions.
NEURODIRECT™ KETAMINE CLINICAL DATA IN NEUROPATHIC PAIN
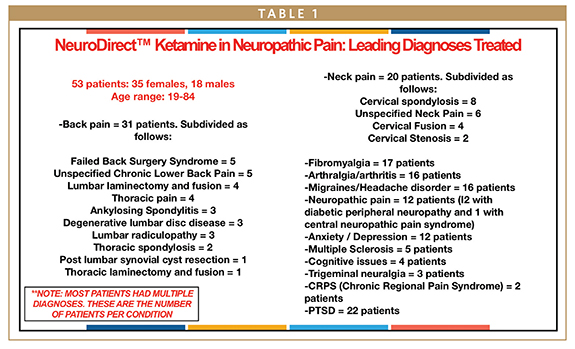
Single doses of NeuroDirect Ketamine 50 mg/ml were studied in 53 consecutive patents presenting to an out-patient General Neurology and Neuropsychiatry practice in Sarasota, FL, with various forms of neuropathic pain and Chronic Regional Pain Syndrome (CRPS). Patients were selected for in-office ketamine treatment based on their diagnoses and symptomatology. Outcome measures to evaluate the efficacy were:
- NUMERIC PAIN SCALE, 0-10, patient self-reported with 0 = no pain; 10 worst possible pain.
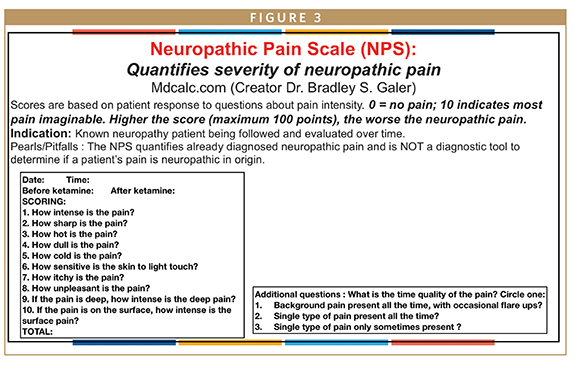
- NEUROPATHIC PAIN SCALE (NPS) (From 0-100. Each category is out of 10 with 10 being the worst pain category. This scale specifically aims to quantify features of neuropathic pain), Figure 3
- HAMILTON DEPRESSION RATING SCALE (Ham-D): multiple-item questionnaire providing indication of depression and treatment response. Self-assessed, with input of family member as corroboration. Designed to rate severity of depression, anxiety, and other symptoms associated with chronic pain syndromes and PTSD; evaluates mood, feelings of guilt, suicide ideation, insomnia, agitation, retardation, anxiety, weight loss, and other somatic symptoms.
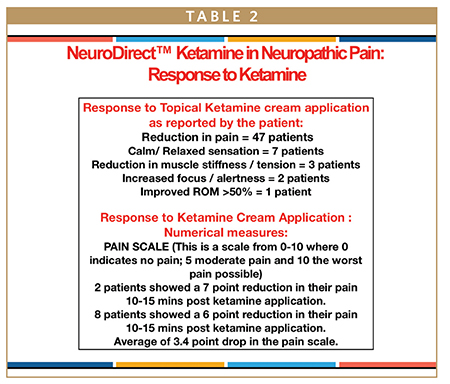
NEURODIRECT™ KETAMINE RESULTS
10-point Pain Scale:
- Pain reduction <10 minutes of application in >88 % patients.
- Average reduction in in all patients: 3.4/10. 7-point reduction in 2 patients; 6-point reduction in 8 patients.
Other areas of improvement after NeuroDirect ketamine:
- Reduction in muscle stiffness and tension: 3 patients
- >50% improved ROM: 1 patient
- More calm and relaxed: 7 patients
- Improved focus and alertness: 2 patients
Neuropathic Pain Scale, NPS (0 to 100 range):
- Average 21.6-point reduction in NPS following ketamine application
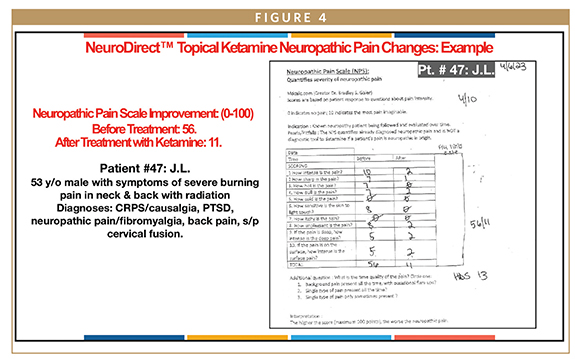
- 54-point reduction in NPS: 1 patient; 46-point reduction in 1; 45-point reduction in 2. (See Figure 4 on patient No. 47: J.L.)
Hamilton Depression Rating Scale, Ham-D (range 0-100):
- A baseline Ham-D on 35 patients: average score 27/100, demonstrating relationship between emotional and physical pain in chronic neuropathic pain states with need for a therapeutic intervention that targets both.
CONCLUSION & PREVALENCE OF NEUROPATHIC PAIN
NeuroDirect Ketamine, previously reported to benefit in management of PTSD is now found beneficial in neuropathic pain. Complex regional pain syndrome (CRPS), is an example of extreme unrelenting widespread form of neuropathic pain with associated vasomotor changes of affected limbs.4,20 Targeting such chronic pain with a fast acting, non-systemic, convenient and easy to use at home NeuroDirect ketamine cream could be of significant benefit in patients with CRPS as well as other neuropathic pain states including chronic neck and back pain.
In 2021, approximately 20.9%, or 51.6 million, of adults in US experienced chronic pain; with 6.9% experiencing intense pain that limited their daily activities, according to CDC.21,22
Chronic pain, or pain that lasts at least 3 months, can be a debilitating condition that affects various aspects of life for many people. It has also been linked to substance use, depression, higher suicide risk and Alzheimer’s disease. “Addressing chronic pain and improving the lives of persons living with pain is a public health imperative,” wrote Rikard and colleagues.22
REFERENCES
- Woolf CJ, American College of P, American Physiological S. Pain: moving from symptom control toward mechanism-specific pharmacologic management. Ann Intern Med. 2004;140(6):441-51.
- Niesters M, Martini C, and Dahan A, Ketamine for chronic pain: risks and benefits, Br J Clin Pharmacol. 2014 Feb; 77(2): 357-367.
- Maher D, Chen L, Mao J, Intravenous Ketamine Infusions for Neuropathic Pain Management: A Promising Therapy in Need of Optimization, Anesthesia & Analgesia 124(2):p 661-674, February 2017.
- Aung-Din, R and Martin, C, NeuroDirect™ Ketamine: Novel, Non-Systemic Topical Therapy for PTSD & Associated Intractable Depression, Drug Development & Delivery. 2023;23(2):32-37.
- Domino EF. Taming the ketamine tiger. Anesthesiology. 2010;113:876-886.
- Petrenko AB, Yamakura T, Baba H, Shimoji K. The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesth Analg. 2003;97:1108-1116.
- Niesters M, Khalili-Mahani N, Martini C, Aarts L, van Gerven J, van Buchem MA, Dahan A, Rombouts S. Effect of subanesthetic ketamine on intrinsic functional brain connectivity: a placebo controlled functional magnetic resonance imaging study in healthy volunteers. Anesthesioloy. 2012;117:868-877. [PubMed] [Google Scholar].
- Niesters M, Aarts L, Sarton E, Dahan A. Influence of ketamine and morphine on descending pain modulation in chronic pain patients: a randomized placebo controlled cross-over study. Br J Anaesth 2013. [Epub ahead of print] [PubMed].
- Hirota K, Lambert DG. Ketamine: new uses for an old drug? Br J Anaesth. 2011;107:123-126. [PubMed] [Google Scholar].
- Li N, Lee B, Liu RJ, Banasr M, Dwyer JM, Iwata M, Li XY, Aghajanian G, Duman RS. mTOR-dependent synapse formation underlies rapid antidepressant effects of NMDA antagonists. Science. 2010;329:959-964. [PMC free article] [PubMed] [Google Scholar].
- Bowdle AT, Radant AD, Cowley DS, Kharash ED, Strassman RJ, Ray-Byrne PP. Psychedelic effects of ketamine in healthy volunteers. Anesthesiology. 1998;88:82-88. [PubMed] [Google Scholar].
- McRoberts JA, Ennes HS, Marvizon JC, Fanselow MS, Mayer EA, Vissel B. Selective knockdown of NMDA receptors in primary afferent neurons decreases pain during phase 2 of the formalin test. Neuroscience. 2011;172:474-82. doi: 10.1016/j.neuroscience.2010.10.045. [PMC free article] [PubMed] [CrossRef] [Google Scholar].
- Willert RP, Woolf CJ, Hobson AR, Delaney C, Thompson DG, Aziz Q. The development and maintenance of human visceral pain hypersensitivity is dependent on the N-methyl-D-aspartate receptor. Gastroenterology. 2004;126(3):683-92. [PubMed] [Google Scholar].
- Petrenko AB, Yamakura T, Baba H, Shimoji K. The role of N-methyl-D-aspartate (NMDA) receptors in pain: a review. Anesth Analg. 2003;97(4):1108-16. [PubMed] [Google Scholar].
- Parsons CG. NMDA receptors as targets for drug action in neuropathic pain. Eur J Pharmacol. 2001;429(1-3):71-8. [PubMed] [Google Scholar].
- Bennett GJ. Update on the neurophysiology of pain transmission and modulation: focus on the NMDA-receptor. J Pain Symptom Manage. 2000;19(1 Suppl):S2-6. [PubMed] [Google Scholar].
- Sigtermans MJ, van Hilten JJ, Bauer MCR, Arbous MS, Marinus J, Sarton EY, Dahan A. Ketamine produces effective and long-term pain relief in patients with Complex Regional Pain Syndrome Type 1. Pain. 2009;145:304-311. [PubMed] [Google Scholar].
- Woolf TF, Adams JD. Biotransformation of ketamine, (Z)-6-hydroxyketamine, and (E)-6-hydroxyketamine by rat, rabbit, and human liver microsomal preparations. Xenobiotica. 1987;17:839-847.
- Prescribing Information, including Boxed WARNINGS, and Medication Guide for SPRAVATO®, Janssen Pharmaceuticals, Inc. 2023.
- Stanton-Hicks M. Complex regional pain syndrome: manifestations and the role of neurostimulation in its management. J Pain Symptom Manage. 2006 Apr;31(4 Suppl):S20-4. doi: 10.1016/j.jpainsymman.2005.12.011. PMID: 16647591.
- Bascom E, 1 in 5 adults in US has chronic pain, healio.com/news, April 26, 2023.
- Rikard SM, et al. MMWR Morb Mortal Wkly Rep. 2023;doi:10.15585/mmwr.mm7215a1.

Dr. Ronald Aung-Din practices General Neurology & Neuro-Psychiatry in Sarasota, FL. He attended the University of Texas Southwestern Medical School, Dallas, TX, followed by residencies in Neurology and Neurosurgery at University of Florida. He has participated in over 60 pharmaceutical industry-sponsored clinical trials, functioning as Principal Investigator in drug research studies. He is also active in treating varied neurological and psychiatric conditions using delivery of CNS-active drugs with Neuro-Direct™ technology, for which 13 US and foreign patents have been granted to date. AfGin Pharma, LLC was founded in 2009 to advance the unique nature of this non-systemic drug delivery and its goal of Enhanced Neuro-Therapeutics through Direct Effects Topical Technology.

Dr. Chantelle G. Martin iwas born in Zimbabwe, Africa, and attended Medical School at the University of the Free State, Bloemfontein, South Africa, earning her Bachelor of Medicine and Bachelor of Surgery in 2016. She later completed 2 years of internship training at Grey’s Hospital, Pietermaritzburg, South Africa; as well as a year of rural community service. She is currently in the midst of her Internal Medicine residency in the Atlanta, GA, area.
Total Page Views: 10437