Issue:March 2020
CONTAINER CLOSURE INTEGRITY - Mitigating Risk in Pharmaceutical Manufacturing With Visually Inspected Components
ABSTRACT
Final drug products are 100% visually inspected for particulate matter and defects. The aim of visual inspection is to remove defected units. Prevention of these defects should also be an important consideration. The use of visually inspected container closure components can significantly decrease the number of end-of-line rejects associated with these defects, improving the yield and ultimately patient safety. Visible particles and manufacturing defects of the packaging components are discussed here as well as the impact these defects can have on container closure integrity and functional characteristics.
INTRODUCTION
Final parenteral drug products (DP) are required to be essentially free of visible particles; as such they are subject to 100% visual inspection. However, no regulatory requirements are currently applied to the level of particles in primary container closure components.1 Primary container closures must: (a) adequately protect and be compatible with the DP; (b) utilize materials that are safe for use with the DP and the route of administration; and (c) function properly. The primary container closure plays an essential role in the quality of the final DP. The earlier the primary container closure is selected in the drug development process, the easier it is to ensure that DP will not have packaging compatibility issues in the future. Manufacturing defects in container closure components and loose or embedded visible particles can lead to sterility failures and loss of container closure integrity (CCI). In prefilled syringes and cartridges, these defects might also affect functionality. The use of visually inspected container closure components can decrease the risk of a defective final parenteral DP being administered to a patient. Moreover, the overall quality of the final DP will be improved as the final product can only be as good as its components.
Rejection of defective parts is the primary goal of visual inspection. Adoption of automated inspection, at both container closure component manufacturer and DP manufacturer, enables 100% visual inspection, the goal of which is, of course, zero defects. Use of automated visual inspection also enables process control optimization; this enables continuous feedback to the manufacturing process with the result of reduced reject rates.
United States Pharmacopeia (USP), European Pharmacopoeia (EP), and Japanese Pharmacopoeia (JP) require that final parenteral DP should be free from readily seen visible particles. Visible particles are a common cause of audit observations and findings and one of the leading reasons for parenteral DP recalls. Almost one half of the recalls in sterile DP in 2010-2017 were due to the presence of visible particles.1,2 The use of visually inspected components adds to the control strategy for preventing visible particles. DP recalls put patients at risk and cause shortages. They also impair the financial situation of the company and its position in the marketplace. These recalls can be minimized by placing proper controls on processes, equipment, and procedures. Defects in the primary container closure components can range from critical to minor; classification is based on their effect on CCI and ultimately impact to patient safety. Defects can include, but are not limited to, presence of particles and fibers, cosmetic issues, intermixing (ie, presence of wrong product), and manufacturing defects (eg, issue with product forming or inadequate compounding).
Nonconformities in elastomeric components and aluminum seals are detailed in the Parenteral Drug Association (PDA) Technical Report No. 76.3 Nonconformities in glass vials, cartridges, syringes, and ampoules are detailed in the PDA Technical Report No. 43.4 Both PDA reports serve as excellent guides on defects for which visual inspection should be made. Defects that can negatively impact CCI are considered critical. Their impact depends on both the defect severity and location. Defects on areas responsible for sealing (on vials, syringes, or cartridges and elastomers) have a higher probability to lead to sterility breach and exchange of the vial (or syringe or cartridge) headspace with air and water. Incomplete film coverage on drug contact area of elastomeric component can adversely affect compatibility with the DP.
Some defects can be detected readily during visual inspection and are therefore eliminated at the end of the production line. Other defects cannot be detected readily; they might be located on areas not visible in the final sealed container closure. Others might not be readily detected due to the container closure type (eg, amber or non-transparent containers) or due to the nature of the DP (eg, suspensions or colored liquids).
The following discusses particles and container closure defects, as well as the risks these defects pose to patient safety, CCI, and functionality.
PARTICLES
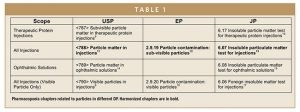
Particles can compromise the quality and safety of parenteral DP and lead to sterility failures. The impact of particles is currently not well correlated to patient harm.5 However, there are requirements for final DP in the USP.6 Chapter USP <1> Injections and Implanted Drug Products (Parenterals) – Product Quality Tests requires that every lot of parenteral DP must be essentially free from visible particles, as defined in USP <790> Visible Particles in Injections.7,8 Subvisible particles are also regulated. Table 1 outlines pharmacopoeia chapters related to particles in different DP.
Particles can be extrinsic (foreign to the manufacturing process, eg, hair, non-process related fibers, etc); intrinsic (from processing or primary packaging materials, eg, stainless steel components, gaskets, packaging glass, and rubber components, fluid transport tubing, etc); or inherent (associated with specific DP formulations, such as suspensions, aggregates, etc) to the final DP. They can be of various sizes and morphologies and can appear in final DP at various concentrations. They can appear during manufacturing, or over time as a result of storage and handling. In particular, they can result from extrinsic sources such as container closure components (for example caused by loose or adhered materials resulting from abrasion/ tumbling).
Quality attributes related to safety, efficacy, potency, and immunogenicity can be affected by particles.18 The identification, classification of size, enumeration, and characterization of particles from all sources are essential for assessing both quality of parenteral DP and impact to patient safety.
While it is important to realize the potential contribution of particles from individual components, the critical particle profile to establish is that of the primary container closure. This can be done only with the final parenteral DP and knowledge of the manufacturing, storage, and shipping conditions. There are well-established container closures for many parenteral DP. However, these can be challenged by specific needs of biologic and cell therapies. For example, the presence of either extrinsic or intrinsic particles formation of protein particles by providing a nucleation site for aggregation. These protein particles can lead to immunogenic responses in patients.18
CONTAINER CLOSURE DEFECTS
Expectations of regulatory agencies is not only that 100% visual inspection will be performed on final DP for the identification and removal of defected products. Since it is well realized that even 100% visual inspection cannot guarantee removal of 100% of defected units (eg, DP with particles present); prevention of defects is important. It is likewise an expectation of regulatory agencies that prevention is pursued. Prevention can be achieved by adopting an inspection life cycle approach. Inspection lifecycle provides a framework for continuous process improvement. It involves multiple elements such as qualification, maintenance, training, and categorization of defects. It also includes testing of components to specific quality attributes and evaluation processes for component preparation and DP filling procedures.19,20 Adoption of 100% visually inspected components helps ensure the prevention of defects and particles appearing in final DP.
CONTAINER CLOSURE INTEGRITY
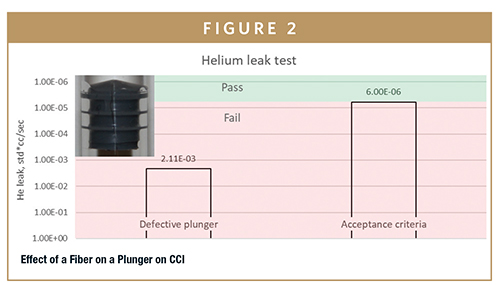
An integral container closure, ie, one with good CCI, prevents microbial ingress, entry of gases and debris, and loss of contents. Quality of container closure components is critical to good CCI. CCI can be negatively impacted by the presence of defects in components, such as cracks, holes, splits, tears, and particles or fibers. An example of a fiber that can negatively impact CCI is shown in Figure 1.

Figure 2 shows a photo of a glass syringe that has a fiber trapped between the plunger and the syringe wall. Tracer gas leak detection with helium was performed on this system – a value of 2.11*10-3std*cc/sec was obtained. This is three orders of magnitude higher than the acceptance criteria for microbial ingress that has been reported by Kirsch, et al.21 This is a clear illustration of the CCI problem that can be caused by a particle.
PERFORMANCE
Defects in syringe and cartridge plungers can cause performance issues, specifically related to functionality and sterility (ie, leakage). Break loose and extrusion forces can increase and become inconsistent, causing administration challenges and negative patient experiences. For autoinjectors and other automated delivery devices, it can cause incomplete dose delivery, or a complete failure if the device cannot overcome increased break loose and extrusion forces. Leakages can cause a breach of sterility and CCI failures. The following performance tests can be used to observe the impact of defects:
-ISO 11040-8 Break Loose and Extrusion Forces and Liquid Leakage Beyond Plunger22
-ISO 13926-2 Freedom from Leakage and Initiating and Sustaining Forces23
-ISO 7886-1 Freedom from Air and Liquid Leakage Past Plunger Stopper and Force to Operate the Piston24
CONCLUSION
Quality of the final parenteral DP depends upon the quality of components, ie, both DP and container closure system. Defective components can result in issues with leakage, contamination, sterility, compatibility with DP, functionality, and machinability. These all pose risk to patient safety. For the final DP, rejection resulting from end-of-line visual inspection may result in drug shortages, along with lower product yields, lost revenue, brand damage, and enhanced regulatory scrutiny. The use of visually inspected container closure components decreases these risks.
REFERENCES
- J. Johns, P. Golfetto, T. Bush, G. Fantozzi, J. Shabushnig, A. Perry, F. De-Grazio, D. Streich, J. Miller, H. Soukiassian, A. Stanton, and R.Watson, PDA J Pharm Sci Technol. 72(6),640-650 (2018).
- J. Shabushnig, M. Lankers, J. Ayres, R. Cherris, R. Miller, R. Veillon, R. Watson, PDA Lett. 54, 20-26 (2019).
- PDA Technical Report No.76, Identification and Classification of Visible Nonconformities in Elastomeric Components and Aluminum Seals for Parenteral Packaging, 2016.
- PDA Technical Report No.43, Identification and Classification of Nonconformities in Molded and Tubular Glass Containers, for Pharmaceutical Manufacturers, 2013.
- S. Bukofzer, J. Ayres, A. Chavez, M. Devera, J. Miller, D. Ross, J. Shabushnig, S. Vargo, H. Watson, R. Watson, PDA J Pharm Sci Technol. 69(1), 123-139 (2015).
- USP, USP 42–NF 37 (United States Pharmacopeial Convention, Rockville, MD, 2009).
- USP, Chapter <1>, “Injections and Implanted Drug Products (Parenterals)—Product Quality Tests”, USP 42–NF 37, 2019.
- USP, Chapter <790>, “Visible Particulates in Injections”, USP 42–NF 37,2019.
- USP, Chapter <787>, “Subvisible Particulate Matter in Therapeutic Protein Injections”, USP 42–NF 37, 2019.
- Chapter 6.17 Insoluble Particulate Matter Test for Therapeutic Protein Injections, Japanese Pharmacopeia 17th Ed, English translation, 2016.
- USP, Chapter <788>, “Particulate Matter in Injections”, USP 42–NF 37, 2019.
- Chapter 2.9.19 Particle Contamination: Sub-Visible Particles, European Pharmacopeia (EP), Eudralex, Ph. Eur. 9th Ed., 2019.
- Chapter 6.07 Insoluble Particulate Matter Test for Injections, Japanese Pharmacopeia 17th Ed, English translation, 2016.
- USP, Chapter <789>, “Particulate Matter in Ophthalmic Solutions”, USP 42–NF 37, 2019.
- Chapter 6.08 Insoluble Particulate Matter Test for Ophthalmic Solutions, Japanese Pharmacopeia 17th Ed, English translation, 2016.
- Chapter 2.9.20 Particulate Contamination: Visible Particles, European Pharmacopeia (EP), Eudralex, Ph. Eur. 9th Ed., 2019.
- Chapter 6.06 Foreign Insoluble Matter Test for Injections, Japanese Pharmacopeia 17th Ed, English translation, 2016.
- E. Moussa, J. Panchal, S. M. Balakrishnan, J. Blum, M. Joubert, L.O. Narhi, E.M. Topp, J Pharm Sci. 105(2), 417–430 (2016).
- R.T. Cherris, PDA Visual Inspection Forum (Bethesda, MD, 2011).
- USP, General Chapter <1790>, “Visual Inspection of Injections”, USP 42–NF 37, 2019.
- L.E. Kirsch, L. Nguyen, C.S. Moeckly, R. Gerth, PDA J Pharm Sci Technol. 51(5),195-202 (1997).
- ISO 11040-8 Prefilled syringes. Part 8: Requirements and test methods for finished prefilled syringes (2016).
- ISO 13926-2 Pen systems. Part 2: Plunger stoppers for pen-injectors for medical use (2017).
- ISO 7886-1 Sterile hypodermic syringes for single use. Part 1: Syringes for manual use (2017).
To view this issue and all back issues online, please visit www.drug-dev.com.

Dr. Olga Laskina is Senior Technical Account Specialist at West Pharmaceutical Services, supporting customers in technical matters related to product and packaging development, drug-closure compatibility, packaging recommendations, packaging component processing, drug-closure compatibility testing, extractables and leachables, particle analysis, container closure integrity, device functionality, self-injection systems, and reconstitution & transfer systems. She earned her BS in Chemical Engineering for Saint Petersburg State Institute of Technology and her PhD in Chemistry from the University of Iowa.
Total Page Views: 7606