Issue:June 2022
BIORESORBABLE POLYMERIC MATRICES - Convergence of Materials Science & Drug Development to Treat Challenging ENT Diseases
INTRODUCTION
Sustained and controlled delivery of medicine offers important benefits in terms of longer duration of action, reduced dosing frequency, and improved patient comfort and compliance. Several strategies are available to modify release of active substances with a goal of improving patient outcomes; however, these strategies are not applicable to all diseases or areas of the body for delivery, leaving significant unmet needs. For example, it has been challenging to achieve local therapeutic action at tissues deep in the ear, nose, and throat (ENT) passages where inflammation and infection are the drivers of chronic symptoms.
Polymeric microspheres have been used for years for controlled delivery because of their ability to encapsulate different types of drugs, biocompatibility, high bioavailability, and sustained drug release characteristics.1 While microspheres remain an important option for sustained delivery, therapeutic applications are limited to those requiring systemic distribution of the drug. Strategies to localize sustained drug release include the use of foams impregnated with drug product. An example of this approach is a foam-based extended-release formulation of ciprofloxacin for use in ear infections.2 While this once-daily dosing of foam eliminates the need for multiple doses of messy ear drops, use of foams has not been demonstrated to achieve long-term delivery of a therapeutic to a target organ.
Drug-eluting stents (DESs) are drug-device combinations deployed to localize drug delivery in the treatment of obstructive arterial disease. These stents consist of three main parts: a metallic platform, a polymeric coating, and an active pharmaceutical agent incorporated into the coating.3 High rates of in-stent restenosis associated with bare-metal stents led to development of DESs, which were designed to mitigate the injury created by implantation of the stent.4 In other words, the goal of the drug in DESs is to make the device – the stent – work better.
As our research team explored ways to deliver drugs and treat disease in a targeted, long-term manner for specific ENT conditions, we sought to move beyond the limitations imposed by technologies such as microcarriers and foams. At the same time, we envisioned an approach that was, in essence, the reverse of a DES. We didn’t look for a drug to make an existing device better, rather, we wanted to develop an implantable material with a specific set of characteristics that offered the potential to make a broad range of therapeutics more effective.
We ultimately found a unique way to solve a unique problem at the intersection of material science and drug formulation chemistry.
CHECKING ALL THE BOXES
When considering an advanced material and design for an implant capable of localized, long-term delivery of a therapeutic, the list of prerequisites is lengthy. As a starting point, we considered the nature of the soft tissues we would be targeting and knew the implants needed to mimic the strength and elasticity of the native tissue and also have shape-memory properties. These features would allow the implant, and hence the drug, to remain in contact with the tissue surface even as the tissue changes and remodels. The implant material also had to be resorbable and biocompatible.
Development of a shape-memory material that is also bioresorbable required a unique composite design as existing approaches offered limited strength. The bioresorbable, composite polymeric implants with shape-memory properties that Lyra has developed are described in Nature Materials.5
The shape-memory matrix consists of variants of poly(glycolic) acid that are braided and coated with a crosslinked elastomer of poly(glycolide-co-caprolactone). The elastomer coating delivers higher mechanical strength in terms of compression, expansion, and elasticity compared to braids without the coating. The elastomer is cured on the braid at the fully expanded diameter, providing a mechanism for the implant to self-expand to its fabricated diameter by constraining the points of intersection of the braid. The scaffolds were shown to be biocompatible and highly resorbable in animal studies.
This novel approach to coupling strong materials with elastomeric, shape-memory materials opened the opportunity for the long-term targeted delivery of drugs via bioresorbable constructs that mimic the properties of native soft tissue.
THERAPEUTIC APPLICATIONS
At Lyra Therapeutics, we have integrated this technology based on advanced materials science with extensive expertise in drug development and formulation chemistry to create our XTreo™ platform. Foundational components of the XTreo platform are outlined below.
A biocompatible mesh design optimizes surface area for drug release while maintaining underlying tissue function through an open cell design. The mesh is composed of bioresorbable polymers that are pliable to maximize patient comfort.
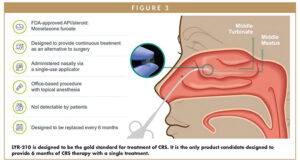
An engineered elastomeric matrix (Figure 1) dynamically adapts to target anatomy. Adaptive elastic tension gives it shape-memory to resist deformation, which is essential for ensuring persistent positioning in the target location. The elastomeric matrix works in conjunction with the underlying mesh to exert out- ward pressure at the target location, keeping it in place as tissue remodels. Resorption of the matrix can be con- trolled to effectively tailor the therapeutic to different indications; it can be designed to remain intact or be resorbed within a specific time period. A fine-tuning process effectively balances the pace of resorption and self-expansion.
A versatile polymer-drug complex is potentially amenable to continuous, prolonged drug release across a wide range of drugs for different therapeutic applications. With proprietary bioresorbable polymer-drug formulations, the platform can be used to customize the controlled-release of drugs for many chronic diseases.Our current pipeline of therapeutics target tissues deep in the ear, nose, and throat (ENT) passages and are designed to deliver continuous drug therapy for up to 6 months following a single non-invasive, in-office administration.
TARGETING CHRONIC RHINOSINUSITIS
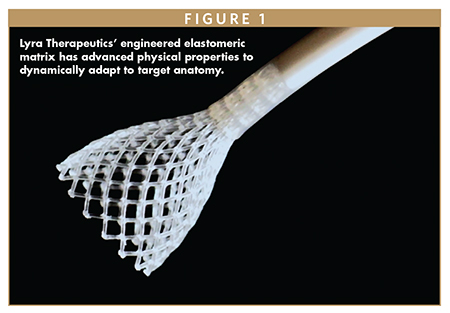
Selection of chronic rhinosinusitis (CRS) as our first indication was driven by significant unmet clinical need (Figure 2). CRS is one of the most prevalent chronic diseases, affecting at least 14 million in the US alone.6 CRS is diagnosed after persistent and severe symptoms, which include nasal congestion, drainage, reduced or lost sense of smell, and facial pain and pressure, have persisted for 3 months or more. CRS symptoms can lead to sleep disturbances, daytime fatigue, depression, and anxiety, severely impacting a person’s well-being and quality of life, both personally and professionally. A typical CRS sufferer misses 18 workdays per year, has a 36% reduction in on-the-job effectiveness, suffers a 38% loss of productivity, and often withdraws from daily personal activities.7
Conventional CRS treatments are intended to reduce mucosal swelling resulting from underlying inflammation, reduce existing nasal polyps and promote sinus drainage. CRS sufferers typically start with over-the-counter remedies and if those don’t work, may move to a topical intranasal or oral corticosteroids. Topical nasal steroid sprays are not designed to reach the site of inflammation deep within the nasal passages, and systemic exposure to oral steroids also presents safety concerns for these patients.
About 10% of CRS patients develop nasal polyps, which are benign, tear-shaped masses that form in sinus cavities. Currently, there are no FDA approved drug therapies for the 90% of CRS patients who do not have polyps.
Overall, 50% of the 8 million CRS patients in the US fail attempts to manage CRS with medication.8 These patients may be referred for sinus surgery, which can be costly and uncomfortable. A small minority of patients proceed with sinus surgery, and those that do often require follow-up revision surgeries. The majority of CRS patients still require medical management after surgery.
The unmet need in CRS is significant as none of the current treatment options offer the sustained solution required for long term management of this disease.
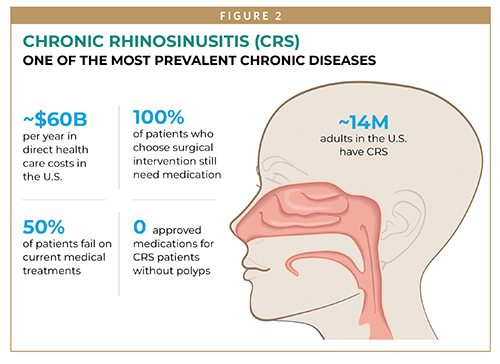
LYR-210 is an anti-inflammatory implantable drug matrix based on our XTreo platform designed to deliver mometasone furoate, a potent anti-inflammatory agent, consistently and locally to the inflamed mucosal tissue of patients with CRS for up to 6 months from a single treatment (Figure 3).
In the Phase 2 LANTERN study, LYR-210 demon strated rapid and durable improvements in symptom severity for patients both with and without nasal polyps after a single ad ministration. At 4 weeks, 70% of patients showed clinically meaningful improvement, and by 24 weeks 100% of patients achieved meaningful symptom improvement. Furthermore, approximately 50% of CRS patients treated with LYR-210 experienced durable symptom improvement 6 months after removal of the matrix. The lack of a strong rebound in CRS symptoms post-treatment after removal of the matrix may indicate the potential for longer-term benefit for some patients.
Another long-acting anti-inflammatory implantable drug matrix, LYR-220, is in development for CRS patients who have undergone a prior sinus surgery but continue to have persistent disease. Sinus surgery results in an enlarged nasal cavity, and LYR-220 employs an oversized matrix to ensure a proper fit.
An applicator designed for the specialized biology and contour of the ENT space is used by the physician to administer LYR-210 and LYR-220 in a fast, non-invasive, in-office procedure. The flexible matrix maintains maximal contact with the irregular sinonasal anatomy and dynamically expands to the target anatomy, promoting continuous apposition to the surrounding mucosa for efficient and consistent local corticosteroid delivery while being unobtrusive to patients.
SUMMARY
The XTreo platform represents a unique and powerful convergence of materials science, drug development, and formulation chemistry, enabling the local delivery of medication to anatomical spaces not accessible by conventional therapeutic approaches. The remarkable flexibility of the platform opens possibilities to explore additional indications within the ENT space, such as allergic rhinitis, olfactory dysfunction, ear conditions, and sinus-related rare disorders. Because this versatile platform enables modification of the form factor, the drug and its elution profile, we can explore indications beyond the ENT space as well, such as nasal delivery for CNS disorders. Lyra’s XTreo platform has potential in a number of indications where long-term delivery would improve local bioavailability and enhance efficacy and safety.
REFERENCES
- Varde NK and Pack DW. Microspheres for controlled release drug delivery. Expert Opin Biol Ther. 2004 Jan;4(1):35-51. doi: 10.1517/14712598.4.1.35. PMID:14680467.
- https://www.timesofisrael.com/foam-delivery-to-make-earaches-less-of-a-headache-for-parents/.
- Rykowska I, et al. Drug-Eluting Stents and Balloons—Materials, Structure Designs, and Coating Techniques: A Review. Molecules 2020 25:4624. doi:10.3390/molecules25204624.
- Shlofmitz E, et al. Restenosis of Drug-Eluting Stents: A New Classification System Based on Disease Mechanism to Guide Treatment and State-of-the-Art Review. Circulation: Cardiovascular Interventions. 2019 12(8). https://doi.org/10.1161/CIRCINTERVENTIONS.118.007023.
- Sharma U, et al. The development of bioresorbable composite polymeric implants with high mechanical strength. 2018 17:96-103. DOI: 10.1038/NMAT5016.
- DeConde AS, Soler ZM. Chronic rhinosinusitis: Epidemiology and burden of disease. Am J Rhinol Allergy. 2016 Mar-Apr;30(2):134-9. doi: 10.2500/ajra.2016.30.4297. PMID: 26980394.
- Fokkens WJ, Lund VJ, Hopkins C, et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinology. 2020 Feb 20;58(Suppl S29):1-464. doi: 10.4193/Rhin20.600. PMID: 32077450.
- Baguley et al. The fate of chronic rhinosinusitis sufferers after maximal medical therapy. Int Forum Allergy Rhinol, 2014 4(7):525-32.

Dr. Maria Palasis is President and Chief Executive Officer of Lyra Therapeutics. She is an accomplished scientist, inventor, entrepreneur, and healthcare industry leader who has led the development of multiple highly successful medical device and drug delivery systems. She is considered one of the pioneers of drug-eluting stents, currently over a ~$6B annual commercial market, and she led Lyra through its successful initial public offering in May 2020 – one of the first IPOs after lockdown for the COVID-19 pandemic. She was elected into the National Academy of Engineering for outstanding contributions to the design of medical devices and drug delivery systems, including her work on LYR-210 and LYR-220. She earned her PhD in Chemical Engineering from the University of Cincinnati, Collge of Engineering & Applied Science.

Dr. Robert Kern is Chief Medical Officer of Lyra Therapeutics and the George A. Sisson Professor and Chair, Department of Otolaryngology – Head and Neck Surgery, Northwestern University Feinberg School of Medicine. He has 30 years of experience in the ear, nose, and throat field and is a practicing otolaryngologist with a subspecialty interest in rhinology. He is the immediate Past President of the American Rhinologic Society and current President of the International Society of Inflammation and Allergy of the Nose.
Total Page Views: 5014