Issue:June 2018
ANTIBODY DISCOVERY - Why Understanding Immune Dysregulation is the Key to Drug Development
ABSTRACT
Antibodies have been used since the late 1980s as therapies to treat serious diseases, and demand is soaring to new heights today. However, conventional antibody drug discovery technologies are labor-intensive and slow. Pharmaceutical companies select drug candidates from just a small fraction of the antibodies that exist in a natural immune repertoire and have limited information on which candidates are the most promising. Additionally, identification and selection of drug targets remain an arduous process because conventional approaches to studying the immune system are not comprehensive. GigaGen Inc., based in South San Francisco, CA, has developed a unique insight into immune dysregulation through a proprietary technology known as Surge – a platform that quickly characterizes every cell in complex immune systems so that natural immune repertoires can be translated into medical treatments. The technology powers selection of drug targets, identification of drug candidates, and preclinical assessment of efficacy. GigaGen is using their insight into how the immune system functions to discover and develop drugs that solve disorders of immune dysregulation, including cancer and immune deficiency.
INTRODUCTION
Cancer. Rheumatoid arthritis. Primary immune deficiency. These and many more of the world’s most devastating and widespread diseases involve dysregulation of the immune system. The body’s network of cells, tissues, and organs that are designed to keep us healthy either fails to properly react against a dangerous “invader,” or it over-reacts. In either case, the result is disease — and it can be deadly.
Fortunately, throughout the past 3 decades, modern medicine has made great strides in treating dozens of immune-based conditions using antibody therapeutics. In the past 2 years alone, more than 20 of these drugs have gained FDA approval. Market research firms have estimated the global market for monoclonal antibodies at $85.4 billion in 2015, and expect it will soar to a value of $138.6 billion by 2024.
Since the human genome was sequenced, the number of well-characterized antibody targets has exploded. In particular, the field of cancer immunology has expanded rapidly. Antibodies targeting PD-1 and CTLA4 are among the most successful new cancer drugs in decades. These “checkpoint inhibitor” drugs specifically activate the immune system to target and kill tumor cells. At GigaGen and elsewhere, new insights into the tumor microenvironment continue to drive discovery of new checkpoint inhibitor targets. There is tremendous competition to quickly turn these novel insights into drug pipelines.
However, immune systems are incredibly complex and still poorly understood. Immune cells respond to hundreds of stimulatory and inhibitory proteins, and constantly change during sickness and health. To understand immune systems, drug companies and academic researchers perform millions of cellular bioassays every day. Conventionally, studies of cell-cell interactions are performed in tissue culture plates, often on large, bulk populations of hundreds of thousands of cells rather than pairs of single cells. To scale these kinds of assays, drug companies and academics typically either severely reduce the ambition of their projects or spend millions of dollars on robotic automation. Eliminating this bottleneck could help unravel complex biological pathways, identify new targets, and eventually bring new innovative drugs to market.
Furthermore, once drug targets are identified, it’s simply not good enough to have a single antibody against a single target in hand, which becomes the case when in-licensing from academia, for example. This is due to antibodies varying enormously in quality. In the checkpoint inhibitor field, for instance, a higher-affinity antibody is not necessarily a better drug choice. To block or activate immune receptors, antibodies must bind to the correct part of the target, and often the correct part of the target is not known upfront. Additionally, to avoid toxic side effects, antibodies must not bind non-specifically. On the other end of the spectrum, if an antibody binds too strongly to the correct target, there are also significant toxic side effects.
To build robust drug pipelines, most antibody drug discovery methods leverage mouse hybridomas. In this process, mice are immunized with a checkpoint inhibitor target and hybridomas are created from mouse B cells. However, this process is so inefficient that less than 1% of the original B cell diversity is retained. To compensate, large pharmaceutical companies have built massive, expensive robotic facilities. Still, discovery using this method requires years of effort. Small companies, on the contrary, lack hundreds of millions of dollars to build robotics and typically must choose a single target. They then will spend tens of millions of dollars to build a portfolio they hope will become competitive with large pharmaceutical companies.
WHEN CURRENT TECHNOLOGY IS LACKING, INNOVATE
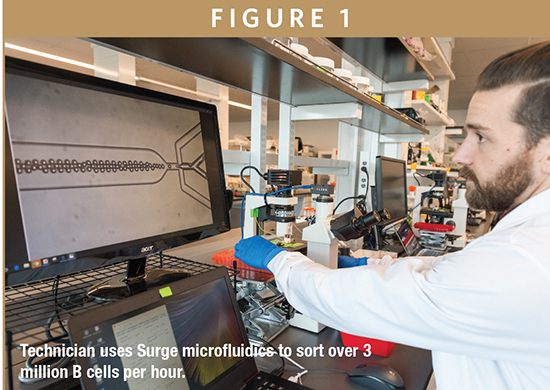
Innovation is an alternative to spending large amounts of time and money on capital equipment. At GigaGen, we built an ultra-fast, ultra-efficient technology that characterizes every cell in complex immune systems, accelerating the selection of drug targets, identification of drug candidates, and preclinical assessment of drug efficacy. We call this technology Surge, and it leverages modern advances in microfluidics and genomics (Figure 1).
For target discovery, Surge is a method for massively parallel bioassays in picoliter droplets. We are able to study millions of cellular interactions, revealing changes in proteins that regulate the immune system. This facilitates discovery of novel pathways for modulating immune dysregulation, including genes that are involved in dysregulation of T and B cells. These genes may one day become novel drug targets. Previously, researchers might have incubated immune cells and their targets in 96-well plates, and then assayed cellular responses through methods such as flow cytometry, ELISA, or ELISpot. Such technologies are poorly suited for combinatorial analysis, for example, screening a millions-diverse panel of antibody-secreting cells against a millions-diverse panel of target cells. Thus, researchers using conventional technologies are forced to study only a few antibodies and targets at a time, severely constraining forward progress.
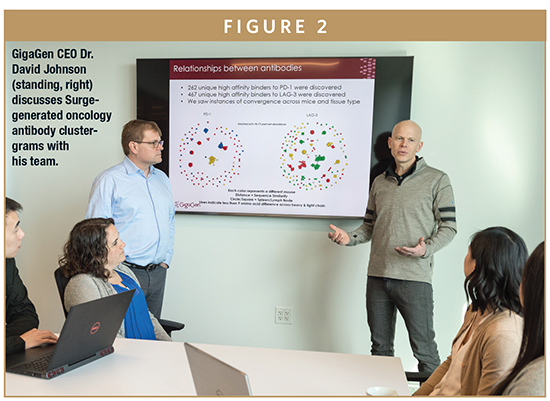
For antibody drug discovery, we immunize mice with an antibody target of interest. Then, we run the mouse B cells through our microfluidic platform to capture antibody sequences on a single cell level, but millions at a time. This process turns the efficiency of hybridomas upsidedown, achieving more than 99% efficiency rather than less than 1% efficiency. We therefore mine for, and find, antibodies that no other technology is able to (Figure 2). Many of these antibodies could end up being the most efficacious or safest antibodies. The Surge technology is also proving to be much faster than conventional hybridoma technologies. Hybridoma screening involves several steps of assaying hybridoma pools, followed by single-cell cloning and expansion, finally followed by sequencing – a process that takes many months, or even years. The process we utilize with Surge determines the sequences of high affinity antibodies within days, allowing us to spend more time and financial resources on biological characterization and antibody optimization.
Though Surge works quickly, it took years to develop. GigaGen was founded in 2011 by myself and a Stanford colleague and immunology professor, Dr. Everett Hurteau Meyer. We have been supported by more than $10 million in NIH grant funding from the National Cancer Institute and the National Science Foundation and have generated numerous patent filings related to single cell droplet immune genomics, with the first issued patents in Europe and the United States in 2016.
In 2017, we published our work on mouse repertoires in the journal mAbs. We immunized wild type mice with the checkpoint target PD-1 and ran millions of B cells through our microfluidic system. We discovered hundreds of high-affinity PD-1 binders in only five mice in less than a month and utilizing only a single technician. These antibodies were often very rare, present at less than 0.01% of the original B cell repertoire. Even with the benefit of automated robot screening, hybridoma methods would have likely missed many of these rare antibodies. We examined 17 of the most promising antibodies in more detail and found nine antibodies that showed efficacy using our in vitro cellular assays. We are now performing affinity maturation in vitro on these antibodies for further non-clinical development.
The speed and convenience of our method results in a larger number of candidates for development pipelines. More mouse – or human – repertoires can be screened and this screening process can be conducted more exhaustively. This has substantial advantages for intellectual property because a program can choose a target and quickly identify hundreds of unique, validated binders. In theory, technologies such as Surge could also lead to shorter commercialization timelines.
We have also used our technology to discover rare, high-affinity binders in human repertoires, which was also highlighted in the journal mAbs in 2017. In this study, we used our microfluidic methods to create a large library of antibodies from the B cell repertoires of 52 healthy human donors. Yeast technology was then used to screen the library for binders against pneumococcus and influenza A antigens. Again, we found hundreds of high-affinity antibody binders – some as rare as 0.001% frequency in the original library. We followed up with efficacy assays using 19 of the antibodies. These antibodies had a surprising diversity of functionalities, reiterating the importance of capturing a wide variety of antibodies when developing a robust pipeline.
INSIGHT INTO IMMUNE SYSTEM FUNCTION LEADS TO NOVEL THERAPIES
Using Surge, we have been fortunate to come to understand disorders of immune dysregulation at a level that is unprecedented, spurring development of novel, revolutionary therapies for patients. We are first applying our insight to produce therapies targeting immune deficiency and cancer.
Immune deficiencies are characterized by the body’s inability to properly make antibodies; consequently, patients with immune deficiencies are susceptible to recurrent and severe infections caused by viruses and bacteria that healthy individuals are able to fight off naturally. Patients with immune deficiencies are routinely treated with plasma-based drug products called intravenous immunoglobulin (IVIG), or high-titer variations referred to as “hyperimmunes,” made by pooling Immunoglobulin G (IgG) antibodies from thousands of human donors. The plasma IgG drug industry is a $10-billion industry that has seen little innovation in decades, despite strong demand from doctors who treat immune deficiencies and their patients. Conventional plasma IgG drug products suffer several shortcomings that include constrained supply, risk of contamination by blood-borne pathogens and limited potency.
In our work to treat immune deficiency, we identified vaccinated individuals that were good responders to infection against pneumococcus, haemophilus, and viral influenza through immune repertoire profiling. This finding suggested development feasibility of therapeutics enriched against specific pathogens for patients with immune deficiency. Some of the data were published, and the work led to more than $6 million in funding from NIAID, and a $50-million investment and co-development deal with pharmaceutical company Grifols to develop recombinant polyclonal antibody therapies (Figure 3).
The ability to profile complex immune systems enabled us to develop and complete preclinical validation for the world’s first recombinant polyclonal IgG product, a product that is advantaged over its plasma counterparts in that the risk for contamination from blood-bourne pathogens is exceedingly low. Additionally, both production and batch-to-batch consistency can be controlled through manufacturing, which significantly reduces the risk of limited potency or supply shortage. Similarly, the recombinant nature of the drug enables us to engineer higher potency products than plasma-derived equivalents.
We have also applied our understanding of immune dysregulation to the field of oncology, selecting 17 checkpoint inhibitor targets to create antibodies against. Surge enabled us to immunize chimeric mice that produce fully human antibodies and run hundreds of millions of B cells from these mice through our microfluidic system. In a few months, we have discovered thousands of high-affinity binders to these 17 targets. We have synthesized and purified hundreds of candidates and have shown efficacy using cellular assays. These clinical candidates are all antibodies of natural-repertoire origin, with natural light- and heavy-chain pairing — factors that may increase drug developability and performance.
Our Surge technology and insight into cancer immunology has enabled us to build a highly competitive oncology drug pipeline from nothing, in a matter of months. The diversity of our portfolio gives us the unique ability to test combinations of repressor and activator agonists in vitro and in vivo before going to the clinic. This is critical because we have found through our research that immune repressive pathways can be repetitive, and it is therefore necessary to address multiple targets to avoid tumor escape from immunotherapy.
SUMMARY
At GigaGen, we envision a future in which the only hurdle in drug development is the clinical trial. Our technology has enabled us to build a robust portfolio of checkpoint inhibitor antibodies in a matter of months, and lay the groundwork for recombinant polyclonal IgG drugs poised to revolutionize treatment of immune deficiencies. For the first time ever, it’s possible to understand immune response to disease with incredible breadth and detail and use this power to create life-saving therapies.

Dr. David S. Johnson is CEO and Co-founder of GigaGen Inc. He is an inventor, entrepreneur, and expert in single-cell immunology with a track record of bringing new medical technologies to market. At GigaGen, Dr. Johnson has served as Principal Investigator for 16 grants from NSF, NCI, and NIAID, including seven Phase II projects. These grants led to about $52 million in partnerships with several established pharmaceutical companies, including Grifols, Novartis, and Merck. Prior to GigaGen, Dr. Johnson was among the founding members and COO of Natera, a reproductive molecular diagnostics firm that went public in 2015 (NASDAQ: NTRA). At Natera, Dr. Johnson was responsible for all clinical operations, laboratory research, clinical studies, and clinical product development. Prior to Natera, he was the ENCODE Project Director at the Stanford Human Genome Center. Dr. Johnson earned his BS in Biology from Duke University, his PhD in Genetics from Stanford University, and his MBA from the Haas School of Business at the University of California, Berkeley. Dr. Johnson’s work has been published in many journals, such as Science, Nature Methods, Blood, and mAbs.
Total Page Views: 4655