Issue:January/February 2017
ADVANCED DELIVERY DEVICES - Disruptive Delivery Technology Partnerships Are Key to Pharmaceutical Life Cycle Management
It’s a challenging time for pharmaceutical executives. Facing the dual imperatives of delivering innovative therapies that address unmet patient needs while delivering profitable growth, they are performing a balancing act between two often conflicting objectives – fostering innovation and containing costs. The industry is responding by embracing disruptive technology that can concurrently help on both fronts and also speed time to market for pharmaceutical products and services. According to a Deloitte 2016 industry report, some of this transformation will take the form of more technology deals as the integration of technology and pharma gains traction and accelerates. A key concept in the report: drugs will remain important but will represent a diminishing share of what comes together to deliver an overall outcome.1
Consequently, a well-balanced biopharmaceutical product portfolio now includes a pathway for continual product innovation, such as incorporating a new delivery component. This is expected to lead to a lower-risk product development strategy and greater overall success in the marketplace.
INNOVATION PROPELS PRODUCT LEADERSHIP
Companies including Roche/Genentech and Novartis provide examples of how such product leadership is achieved. The two companies’ success centers on innovation in developing treatments for specific customer groups. Some of their most successful products of the previous 10 years include first-in-class therapies, such as Avastin (bevacizumab), Rituxan (rituximab), Herceptin (trastuzumab), and Gleevec (imatinib). These products have far higher average projected sales than follow-on products. But to maintain this leadership, they also turned their focus to increased patient convenience, with continual support of the customer base and innovative new treatment paradigms to improve the patient experience.
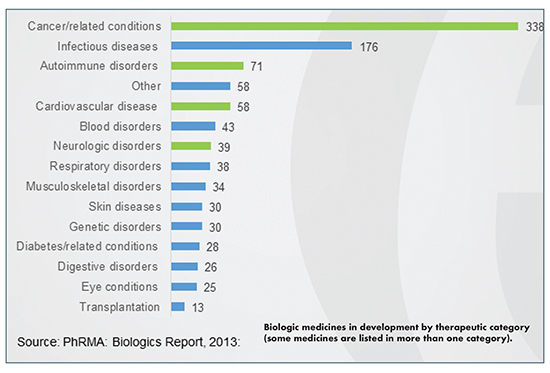
Many other companies are striving for leadership positions for their multiple high-value product franchises. Nowhere is innovation to enhance the patient experience more critical than with the rapidly growing number of high-volume, viscous biologics that now comprise over 50% of products in pharmaceutical development. For these drugs, delivery has been a challenge. But advanced delivery technology specifically developed to replace hospital-based delivery of large-dose drugs is providing new options for creating tomorrow’s patient-friendly blockbusters.
NEW DELIVERY SYSTEMS CAN IMPROVE BIOLOGICS’ BIOAVAILABILITY, ENABLE SUBCUTANEOUS INJECTION
Although progress has been made in the manufacturing of biologics, particularly in the past few years, progress in the development of delivery systems able to improve the bioavailability of biologics has remained rather limited – until now.
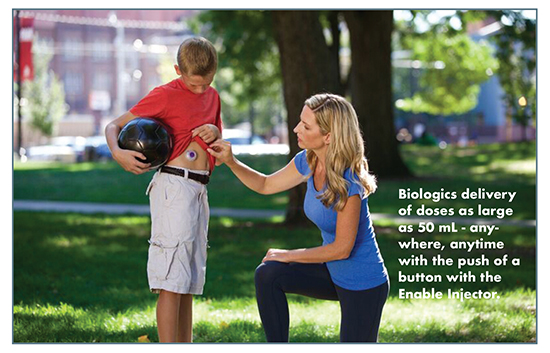
Subcutaneous delivery is generally the preferred way to administer an injectable therapeutic. However, subcutaneous injections have been limited in the amount of drug substance that can be delivered. There are several reasons for this. One of the main concerns in formulation development is the exponential relationship between the concentrations of biologics and viscosity of the formulation. The highly viscous formulations often required to ensure a desired concentration cannot be readily injected.2,3 Generally, the volume of a bolus subcutaneous injection has been limited to no more than 1 to 2 ml. Now advanced delivery technology from Enable Injections can comfortably deliver up to 50 ml subcutaneously with a small wearable device.
For proteins, issues of viscosity, solubility, and protein aggregation are major obstacles, especially with small-gauge needles that patients prefer. For large protein biologics, such as monoclonal antibodies, companies must overcome volume and bioavailability constraints before subcutaneous injections can mirror intravenous-like dosing regimens. Monoclonal antibodies (mAbs) often have high-dose requirements, so they must be formulated at very high concentrations. At low concentrations, an antibody solution’s viscosity increases moderately as a function of protein concentration. But at the high concentrations of some molecules (>100 mg/mL), viscosity increases exponentially.
In addition, concentration to the necessary level in the final product may not be possible for all products because in many cases, upstream purification and manufacturing processes may be the limiting factor in achieving maximum concentration for the final drug product, more so than delivery and fill/finish processes. Finally, drug-product properties, such as pH and osmolality, along with the use of certain excipients, may also limit the most appropriate drug-product concentration. These properties may need to be kept within certain ranges to prevent patient discomfort and injection site reaction.
Several ways to circumvent these volume limitations, including increasing the concentration of the active ingredient in the formulation, are being pursued. While such a change in the administered volume of a drug product offers the ability to deliver a larger dose, this approach can have disadvantages. There are limitations to how rapidly any volume of drug can be injected subcutaneously. The optimal injection time varies greatly by individual drug product. The medical literature regarding the relationship between injection volume and speed is limited. However, it is well known that neither the subcutaneous space — nor patients — can necessarily tolerate rapid injection of larger and larger dose volumes. Tissue disruption and site reaction may occur.
If the injection is rapid and the volume is too large, there is also potential for the product to leak back from the injection site, reducing the bioavailability relative to the total dose. Lastly, the patient may not be able to easily tolerate the rapid injection of a large volume, which could reduce compliance with the therapy. As such, a larger volume of product may require a larger device for self-delivery, and, potentially, a longer injection time.
Understanding subcutaneous tissue pressure is critical for the design of injection devices acceptable to the user. A recent study found that increased pressure and mechanical strain in the subcutaneous space is more directly related to increasing flow rate than to volume.4 Therefore, it is imperative to ensure the user is not inconvenienced during a potentially lengthy administration of therapy.
A potential new solution to large-volume injection challenges is the development and use of systems that administer the dose into the subcutaneous space more slowly. Such systems can expand the possibilities for self-injection.5,6 Due to the need for longer duration of injection, the device or system may need to be temporarily worn on the body at an appropriate injection site, such as the abdomen. Hence, the current industry interest in large-volume wearable injectors (on-body delivery devices).
The rise of viscous biologic drugs, the desired cost-saving shift toward patient self-injection and the emergence of safer, simpler, and more convenient devices are all contributing to the expansion of a new subcutaneous delivery mechanism for the rapidly growing number of large volume, viscous drugs.
ADDRESSING COSTS: ENABLE EASY PATIENT SELF-ADMINISTRATION OF BIG BIOLOGICS AT HOME
On-body delivery systems (OBDS) can be leveraged by a pharmaceutical company to accommodate disparate patient, prescriber, and payer preferences with the potential to improve compliance, build or protect market share, and lower overall health system costs.
The newest, most advanced of these high-volume injectors can move patient treatment from the hospital to the home, reducing costs while at the same time providing the innovator drug company with increased return on investment, and patients with a potentially more favorable treatment option for adherence to chronic and/or maintenance therapies. A time-and-motion study undertaken in eight countries reported significant time-savings for both healthcare professionals and patients through use of subcutaneous rituximab versus intravenous (IV) rituximab. The findings suggest potential for reduced waiting times, greater appointment availability, and improved efficiency of oncology units with the subcutaneous formulation. Subcutaneous injections can also be administered by the patient employing the user-friendly new delivery technology. Such injections are not generally painful and carry a reduced risk of infection and other complications.
Compared with IV drugs, the majority of participants considered subcutaneous drugs clinically safer and more cost-effective, resulting in higher patient satisfaction.7
DISRUPTIVE DELIVERY TECHNOLOGY THAT MERITS RAPID ADOPTION
Wearable injectors are designed to address the challenges of complexity, patient compliance, and cost associated with large-volume subcutaneous injections. The most advanced of these make self-injection safe, easy, comfortable, and convenient for patients – yet cost-effective for the pharmaceutical industry and payers. They bring to market a novel way to cut costs while adding overall value to the healthcare system, resolving drug formulation and delivery challenges by:
-Delivering more volume subcutaneously
-Delivering more viscous, high-concentration proteins subcutaneously
-Offering product differentiation in a competitive market
-Adjusting flow rate to reduce discomfort
-Enabling a simpler, faster method of product preparation
-Utilizing standard vials or syringes to minimize drug stability issues often encountered in new container closure development
-Automatically warming the drug as the injector is filled, thereby removing the typical wait time to use the device for a refrigerated medication
-For lyophilized drugs, completely automating mixing and reconstitution – removing any patient variability from the mixing process
-Using the smallest needle size possible to improve patient comfort
-Designing small wearables with a low profile that can be discreetly worn on the body for greater freedom and mobility
-Incorporating simple data-capture technology to aid in monitoring patient compliance and adherence to therapy
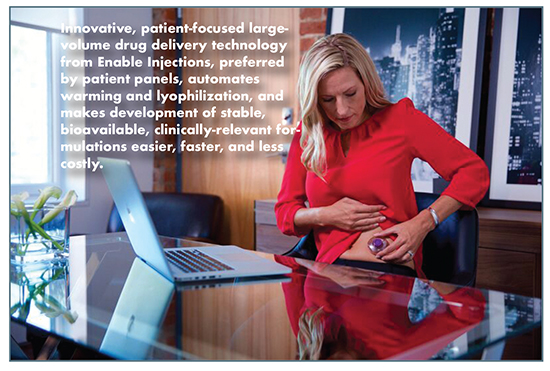
It is of course important to select the right device to deliver the right drug with the right viscosity and the right dose volume over the right period of time. Factors to consider include injection frequency, dose volume, drug viscosity, delivery rate, and duration. Pain, portability, and convenience are also important factors to take into account, which can drive preference rates amongst target patient populations as well as compliance.
With devices becoming increasingly integral to clinical development, regulatory approval, and lifecycle management, pharmaceutical companies should consider newly available drug delivery technology that can differentiate their products and help perform the balancing act between fostering innovation and containing costs. Incorporated data collection capability ensures the effectiveness of the drug delivery innovation by quantifying performance and acceptance of the device as well as optimal dose and flow rate. Such information provides confidence for future development of larger volume biologics for in-home subcutaneous injection. Data will also quickly demonstrate acceptability and likely product uptake, optimizing budgets.
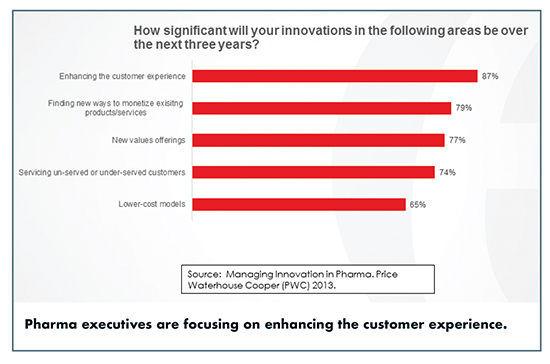
Innovation pays off. A Price Waterhouse Cooper survey of pharmaceutical executives in 13 countries exhorts the industry to innovate beyond just finding new drug candidates – by creative partnering, for example. The PWC study found that returns on effective innovation are “huge.” There was a clear correlation between innovation and growth. The top 20% of innovators anticipated three times as much growth as the bottom 20% in the next 5 years, and a clear majority of pharma C-suite respondents (86%) said innovation is important to their business.8
A large overall pharmaceutical pipeline reported by GBI Research demonstrates that a steady stream of incremental and breakthrough innovation is likely for the foreseeable future for various disease states. With the drugs alone becoming less important, partnering with a disruptive delivery technology could be the key to leadership positioning. Even if it does nothing else, such a partnership will certainly be an option that propels profitable growth by pleasing patients, a winning combination.
REFERENCES
1. 2016 Global Life Sciences Outlook. Deloitte.
2. Collins M. Here’s What’s Important About Alder Biopharmaceuticals Inc (NASDAQ:ALDR)’s Latest Release. Market Exclusive, July 26, 2016.
3. Burgess BE. Optimizing drug delivery for modern biologics. BioPharm Intl. 2012;25(5):30-32.
4. Rule S. Subcutaneous vs intravenous rituximab in patients with non-Hodgkin lymphoma: a time and motion study in the United Kingdom. J Med Econ. 2014;17(7):459-468.
5. Palm T, Sahin E, Gandi R, et al. The importance of the concentration-temperature-viscosity relationship for the development of biologics. BioProcess Int. March 10, 2015.
6. Škalko-Basnet N. Biologics: the role of delivery systems in improved therapy. Biologics. 2014;8:107-114.
7. Doughty D, Clawson CZ, Lambert W, et al. Understanding subcutaneous tissue pressure for engineering injection devices for large-volume protein delivery. J Pharmaceutical Sciences 2016:105:2105-2113.
8. Managing Innovation in Pharma. Price Waterhouse Cooper (PWC), 2013.
To view this issue and all back issues online, please visit www.drug-dev.com.

Michael D. Hooven is President and CEO, Enable Injections, Inc. He has over 30 years of experience in the medical device industry in a broad variety of business, technical, and clinical areas. He is the Founder of five medical device companies and holds over 100 issued and pending US patents. Mr. Hooven is the Founder and a Director of AtriCure, Inc. (NASDAQ:ATRC), where he previously held positions as the Chairman and CEO. He is also Founder and Chairman of Enable Medical, a surgical device manufacturer that was acquired by AtriCure in August of 2005. Prior to Enable Medical, he was Director of Product Development at Ethicon Endo-Surgery from 1988 to 1994, where he had responsibility for all in-house product development and supervised a staff of 200 engineers. He held Engineering positions in pacemaker and lead development at Siemens/Pacesetter from 1986 to 1988 and at Cordis Corporation in neurosurgical products from 1981 to 1986. In addition, he is Director and past Chairman of BioOhio, a state-funded organization to accelerate life-science start-ups in Ohio. He earned his BSc in Physics and a MSME in Mechanical Engineering from the University of Michigan.
Total Page Views: 5569









