Issue:September 2013
THERAPEUTIC FOCUS - New Therapeutics for Aggressive Brain Cancers
INTRODUCTION
In May 2008, Senator Ted Kennedy suffered a seizure, prompting a quick visit to local Cape Cod Hospital, immediately followed by a medical helicopter flight to Massachusetts General Hospital.1 A few days later, on May 20, 2008, doctors reported that a brain tumor caused the seizure. Subsequent biopsy of the tumor tissue revealed that Senator Kennedy had malignant glioma of the parietal lobe. He passed away from the brain tumor 15 months later on August 25, 2009, at his home. The next morning, an NBC headline read: “Kennedy’s tumor was aggressive and deadly. After suffering a seizure last year, the senator battled a malignant glioma.” Indeed the headlines were apt as Senator Kennedy was killed by the most aggressive type of malignant glioma, namely glioblastoma multiforme (GBM) – also one of the deadliest tumors in humans. Even today, despite maximum treatments available, patients still only have median survival times of 15 months. And left untreated, patients will likely succumb to this type of brain cancer in just a few months.
GBM ACCOUNTS FOR MORE THAN HALF OF ALL GLIOMAS
In the US, an estimated 15,000 people have glioblastoma. Of the 25,000 malignant brain tumors diagnosed annually, glioblastoma represents approximately 70%. Gliomas are brain tumors that arise from glial cells, namely astrocytes in GBM, which comprise the supportive “glue-like” tissue of the brain, and they account for over 30% of all primary brain and central nervous system (CNS) tumors diagnosed in the US. GBM is the most malignant and most common, accounting for more than half of all gliomas.
An effective treatment for glioblastoma is needed. Patients with GBM have a median survival of 14.6 months and an overall survival of only 10% at 5 years, even after standard of care (SOC) treatment: surgery, ionizing radiation (IR), and the alkylating chemotherapeutic temozolomide (Temodar®).3
Further, many GBMs have or develop resistance to alkylating chemotherapeutic agents. And while the more recent addition of Temodar (in the mid-2000s) to surgery and radiation therapy has improved survival rates of patients alive after 2 years – from about 10% to 26% – the prognosis today is still grim for glioblastoma.2
RESISTANCE IS A MAJOR PROBLEM WITH TODAY’S STANDARD OF CARE
Generally, tumors of the brain are the most challenging malignancies to treat. Current treatments tend to be aggressive and multifarious. Further, many studies report severaldeterminants of resistance to the current standard of care, such as: (1) O6- methylguanine-DNA methyltransferase (MGMT) expression, (2) the complexity of several altered signaling pathways in GBM, (3) the existence of glioma stem-like cells (GSCs), and (4) the blood-brain barrier.3,4,5,6 Newly diagnosed patients suffering from glioblastoma are initially treated through invasive brain surgery, although disease progression following surgical resection is nearly 100%. Due to the extreme challenge presented to surgeons by these tumors, which can morphologically appear as necrotic hemorrhagic infiltrating masses, and the critical nature of surrounding brain tissue, taking wide margins to include healthy tissue as sometimes is done with other cancers is almost impossible. Thus obtaining clear margins is highly improbable.
Temodar in combination with radiation is the front-line therapy for GBM following surgery. Temodar currently generates more than $950 million annually in global revenues primarily from the treatment of brain cancer. Yet approximately 60% of GBM patients treated with Temodar experience tumor progression within 1 year. This may be due to resistance of the tumors to Temodar, an alkylating chemotherapeutic, especially in those tumor cells that express high levels of MGMT.
MGMT EXPRESSION CAUSES GBM RESISTANCE TO SOME ALKYLATING AGENTS
Many glioblastomas have or develop resistance to alkylating chemotherapeutic agents such as Temodar. One common mechanism of such resistance is mediated by the repair enzyme O6-methylguanine-DNA methyltransferase (MGMT), which is capable of counteracting the anti-cancer cytotoxicity induced by O6-alkylating agents.2 Further, increased MGMT expression is well correlated with in vitro and in vivo glioma resistance to Temodar.4
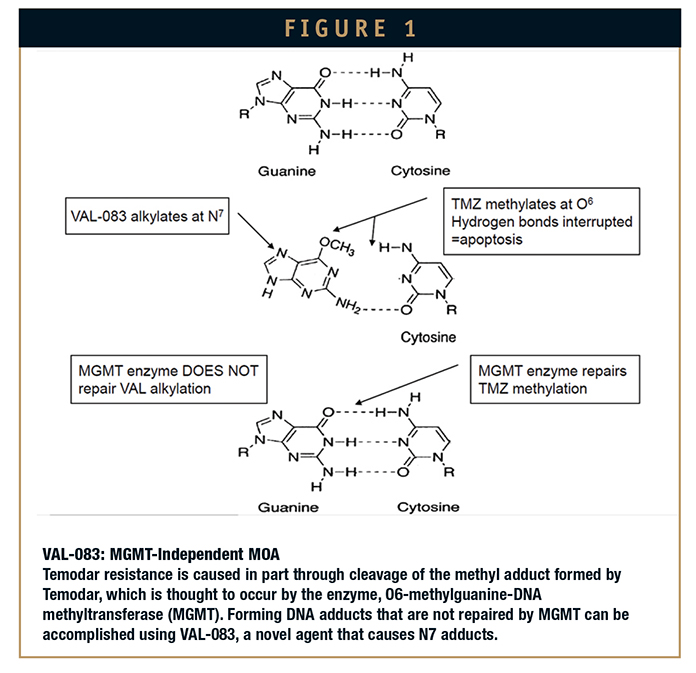
One potential strategy studied for overcoming this resistance is simply administering more frequent Temodar doses in what are referred to as dose-dense or doseintense schedules; however, this has resulted in little benefit in the clinical setting.5 Another strategy is direct enzyme inhibition using O6- benzylguanine, which has been studied in combination with Temodar, but did not yield substantial benefit clincially.6 Therefore, selecting alternate chemotherapeutic agents whose cytotoxic mechanisms are not subject to this MGMT resistance, such as VAL-083 (dihydrogalactitol), may prove to be most beneficial for treatment (Figure 1).
TREATMENT WITH AVASTIN® TARGETING ALTERED VEGF SIGNALING PATHWAY IN PATIENTS FAILING TEMODAR
GBM is characterized by sustained angiogenesis – the key regulator of which is vascular endothelial growth factor (VEGF).4 Bevacizumab (Avastin, BEV) is a humanized monoclonal antibody that binds to and inhibits VEGF. In 2009, the FDA granted approval to bevacizumab injection as a single agent for patients with glioblastoma, with progressive disease following prior therapy.
According to the Avastin label, approximately 20% of patients failing Temodar respond to Avastin therapy. Even with a relatively small patient population, the market for this treatment until recently is still quite large, and analysts anticipate annual Avastin revenues for the treatment of brain cancer may reach $650 million by 2016. Yet interestingly, the Avastin package insert also states that effectiveness in glioblastoma indication is based on improvement in objective response rate – in this case, based both on WHO radiographic criteria and by stable or decreasing corticosteroid use. Further, the label also provides, “No data available demonstrating improvement in disease related symptoms or survival with Avastin.”
In fact, new data from two additional clinical trials on the use of Avastin in glioblastoma presented recently at the annual American Society of Clinical Oncology (ASCO) reveal that Avastin is not a safe or effective choice as a first-line treatment in this indication. And overall Avastin was shown not to have benefit in GBM.
In both studies, Avastin did have a significant impact on progression-free survival (PFS) endpoints, yet it had no impact on overall survival (OS).7 In addition, according to some researchers, using PFS as a primary endpoint is controversial, particularly in patients treated with antiangiogenic therapies (such as bevacizumab) that can lead to improved imaging findings without actual tumor response (a so-called pseudoresponse).4
Also in one study, there was an increase in grade 3 or higher adverse effects in the Avastin arm, including neutropenia, hypertension, and deep vein thrombosis/pulmonary embolism.7 So, as has happened in other indications, such as breast cancer, Avastin is clearly affecting the tumor, but this does not translate to a survival benefit. Approximately 48% of patients who are diagnosed with GBM will fail both front-line therapy and Avastin. Thus, it is clear that new therapeutics are needed to improve the treatment options for patients with glioblastoma, both in first-line and recurrent treatments.
NEW THERAPEUTIC APPROACHES SHOW PROMISE TO TREAT GLIOBLASTOMA
Vaccines & Immunotherapeutic Approaches
Immunotherapy is a promising alternative to conventional treatment for glioblastoma and includes active and passive strategies. Active immunotherapy upregulates an immune response to tumor and can confer long-term immunity that potentially continues to provide protection against future tumor recurrence. Passive immunotherapy involves the transfer of immune effectors to achieve an immediate effect but does not generate long-term immunity.2
Active Immunity: Peptide vaccines seek to induce the immune system to generate a response against the tumor. Of particular interest is a peptide vaccine, known as rindopepimut (CDX-110, Celldex Therapeutics), targeted at epidermal growthfactor receptor variant III (EGFRvIII). This is one of the few identified truly tumor-specific antigens.2 CDX-110 vaccine is currently in several advanced of clinical trials in combination with RT and Temodar.
In particular, CDX-110 is being studied in patients with newly diagnosed tumors that contain the mutation in question in which population it has shown positive results in a Phase II study. It is reported that about 30% of the population has such a variant. Several other promising tumor vaccine strategies are also being used in clinical trials.
Dendritic cells, the immune systems most potent antigen-presenting cells, can be primed with tumor antigen ex vivo and readministered to the patient, where they mediate T-cell activation.8 Numerous preclinical studies demonstrate that dendritic cells pulsed with glioma antigens can prime a cytotoxic lymphocyte response that is tumor specific.2 Thus, immunotherapy with dendritic cells potentially offers high tumor-specific toxicity with sustained tumoricidal activity.9
Of particular interest is a multi-epitopepulsed dendritic cell vaccine, namely ICT-107, being developed by researchers at Cedars Sinai Medical Center.8 The vaccine targets six antigens (HER2/neu, TRP-2, gp100, MAGE-1, IL13Rα2, and AIM-2) involved in the development of glioblastoma cells. Findings from a Phase I clinical trial yielded many interesting results. First, overall survival was 38.4 months, significantly longer than the typical 14.6-month survival of patients with newly diagnosed glioblastoma receiving standard therapy alone, which includes radiation and chemotherapy. Second, patients with tumors that expressed large amounts of MAGE-1, AIM-2, gp100, and HER2 had better immune responses and longer progression-free survival rates, suggesting that these antigens may be particularly vulnerable to the vaccine.
Researchers also reported finding evidence that ICT-107 attacks some brain cancer stem cells, considered by many to be the original source of tumor cells. These selfrenewing cells appear to enable tumors to resist radiation and chemotherapy and even regenerate after treatment. Thus, cancer stem cells are especially appealing targets: killing the stem cells is believed to improve the chances of destroying a tumor and preventing its recurrence. With these encouraging results a Phase II trial is underway.9
Passive Immunity: Antibody-mediated drug delivery serves a dual purpose of increasing the local drug concentration while minimizing systemic exposure. Antibody drug conjugates have been developed that couple monoclonal antibodies targeting gliomaspecific structures to radionuclides (radioimmunoconjugates), exotoxins (immunotoxins), or chemotherapeutic agents and are administrated locally. Antigens that are overexpressed in tumors relative to normal tissue are typically used, such as mutant EGFR, IL-4 or IL-13 receptors.2
Although the benefits of immunotherapy are becoming evident, here and in other fields, substantial breakthroughs supporting its use as the standard-of-care treatment for GBM have yet to be realized. In general, tumors of the CNS pose a distinct set of challenges that may limit the ability to generate an optimal antitumor immune response. Some of these factors include:
• A tight blood-brain barrier that may interfere with localization of immune effectors into the CNS
• Profound immune suppression due to immunoregulatory factors secreted by tumor cells
• A lack of well-defined, tumor-specific antigens for GBM.10
NEW METHODS FOR LOCAL DRUG DELIVERY TO BYPASS BLOOD BRAIN BARRIER
One of the major challenges of chemotherapy for GBM is the achievement of adequate drug concentration within the tumor itself. The blood-brain barrier, although often weakened in areas of bulky tumor, still acts as a barrier against many drugs, particularly in the periphery of the tumor, which is often highly infiltrative.2 The blood-brain barrier is designed to protect the CNS and blocks most anti-cancer drugs, especially molecules that are larger than ∼500 Da. Many drugs are denied access to the very regions where they would be effective, thus limiting the clinical application of most anti-cancer drugs for treating brain tumors So novel methods, such as “superselective intra-arterial cranial infusion” employing microcatheters that when inserted in the groin can be threaded up through tiny vessels almost anywhere in the brain to spray extraordinarily high doses of drugs (some in initial procedures used Avastin) straight to tumors or areas of resection without soaking the rest of the brain in the particular drug and further exposing it, which often results in nasty side effects. For such a procedure, mannitol is first delivered to open up the blood-brain barrier temporarily in order to get chemotherapy in the brain.11
Basically, mannitol pulls water out of the tightly packed cells lining brain capillaries so they shrink and pull away from one another, opening gaps through which drug molecules can pass into the brain tissue. And then the selected drug, in certain studies, Avastin can advance directly to the tumor.
Another novel delivery system utilizes a concept called convection-enhanced delivery, in which surgeons implant one or more catheters into the tumor and the surrounding brain.12 Other chemotherapeutic agents (such as in one particular study with topotecan) are slowly pumped directly into the tumor and surrounding tissue over the course of a few days (e.g. 4 days). Because convectionenhanced delivery is done so slowly, the agent can accumulate in very high concentrations in the tumor, allowing physicians to achieve drug levels more than a thousand-fold greater than is possible with intravenous delivery. Because topotecan is a topoisomerase inhibitor, it affects only multiplying cells such as those in tumors and does not create any additional side effects.
NEW CYTOTOXIC APPROACH WITH MGMT-INDEPENDENT MECHANISM OF ACTION
DelMar Pharmaceuticals has initiated human clinical trials to develop a novel small drug candidate, VAL-083, a chemotherapeutic, that employs a different mechanism of action than presently used chemotherapeutics, such as alkylating agent Temodar. In particular, VAL- 083 employs a mechanism of action seemingly unaffected by MGMT enzyme expression. The enzyme expression triggers the DNA cell repair mechanism that counteracts the cytotoxic activity of currently employed
chemotherapeutics, thus leading to the tumor resistance, which occurs in more than half the GBM patient population. Therefore, VAL-083 effectively addresses the problem of MGMTrelated tumor resistance.
Specifically, VAL-083, as a first-in-class small-molecule chemotherapeutic, has a molecular structure that is not an analogue or derivative of other small molecule chemotherapeutics approved for the treatment of cancer. VAL-083 has been previously assessed in multiple (>40) clinical studies sponsored by the National Cancer Institute (NCI) in the US as a treatment against various cancers, including lung, brain, cervical, ovarian tumors, and leukemia.
Shelved by the NCI, while other drugs and more complex biologic treatments were pursued a number of years ago in the initial front to the war on cancer, VAL-083 was overlooked, until recently. With such a large amount of clinical data available for VAL-083, it has historical and established proven validity in battling cancer. In fact, published preclinical and clinical data suggest that VAL-083 may be active against a range of tumor types.
Additionally, VAL-083 is approved as a cancer chemotherapeutic in China for the treatment of chronic myelogenous leukemia (CML) and lung cancer. VAL-083 has not been approved for any indications outside of China.
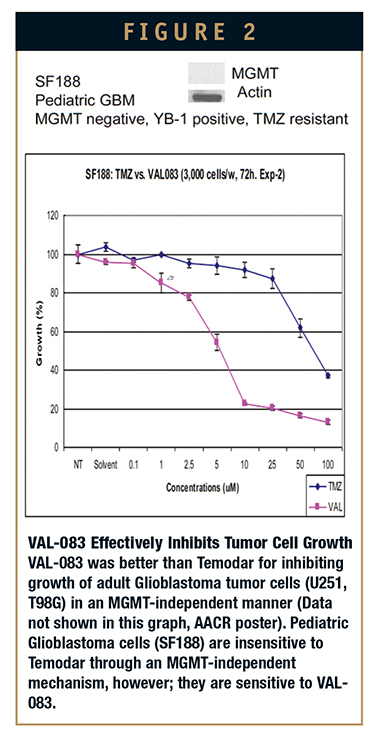
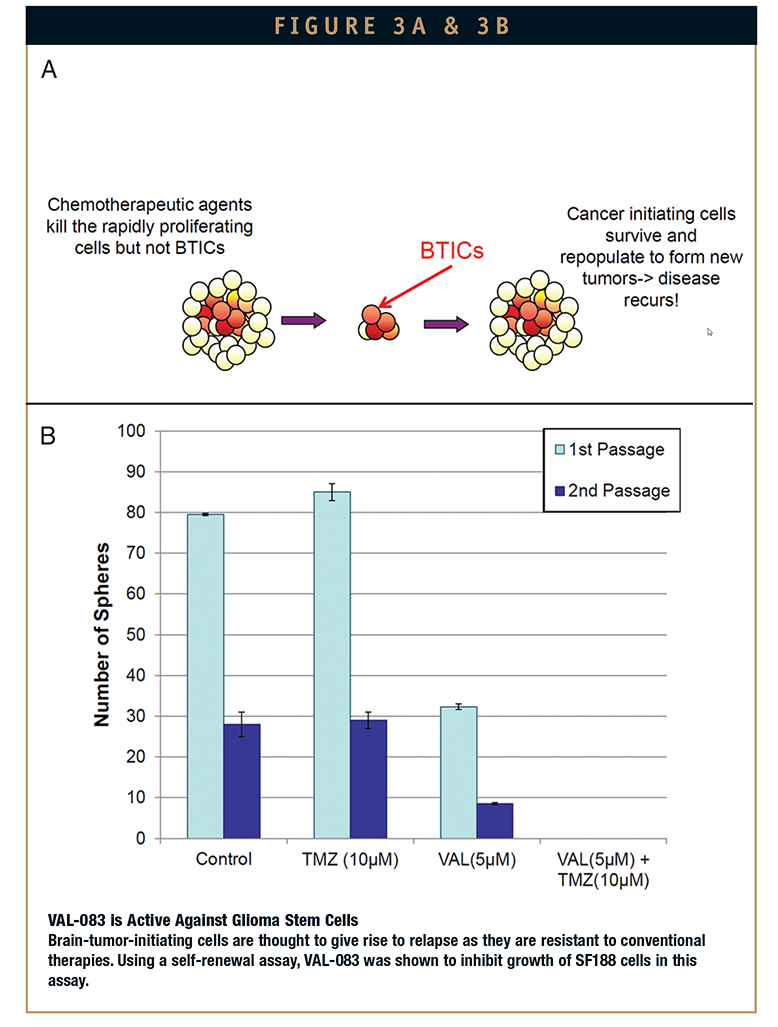
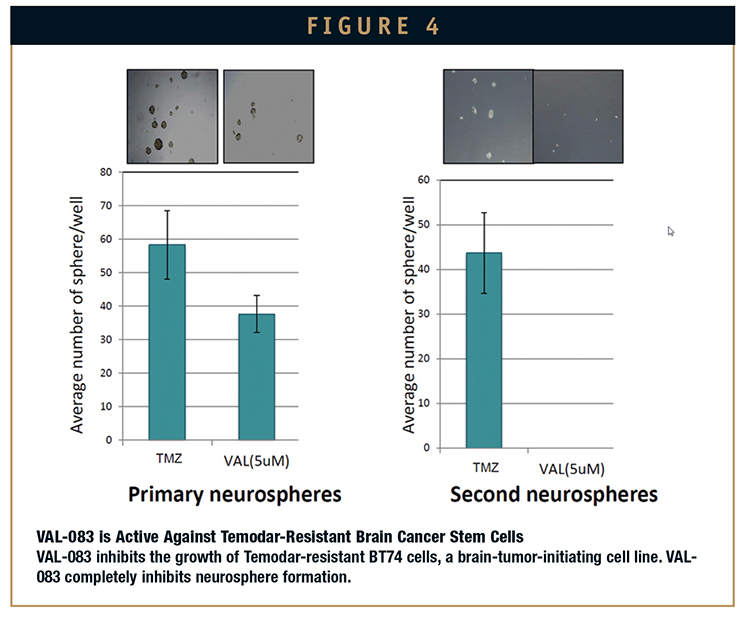
More recently, in October 2011, DelMar Pharmaceuticals initiated clinical trials with VAL-083 as a potential new treatment for GBM. In April 2012, data presented at the American Association of Cancer Research (AACR) annual meeting demonstrated that VAL-083, as expected, maintains activity in tumors resistant to the current front-line GBM therapy, Temodar, due to MGMT-related chemo-resistance (Figure 2). Currently, there is no approved therapy for these patients. DelMar’s data also suggests that VAL-083 is active against glioma stem cells (GSCs) that are resistant to standard chemotherapy (Figures 3 and 4). Further, VAL-083 is safe and well tolerated at doses tested to date.
In November 2012, interim data from a clinical trial was presented at the Annual Meeting of the Society for NeuroOncology (SNO) demonstrating that VAL-083 can shrink or halt the growth of tumors in brain cancer patients who have failed other approved treatments. Most recently, reports continue to confirm the findings of previous studies and potentially position DelMar for advancement to registration trials in early 2014. Specifically, VAL-083 Phase I/II clinical trial interim results that were presented at AACR and ASCO 2013 indicate the following:
• VAL-083 is safe and well tolerated at doses tested to date
• A portion of patients tumors were observed to shrink or stop growing following initiation of treatment
• Benefits were seen in both glioblastoma and in other cancers that have spread to the brain
• Doses to date are lower than NCIregimen, indicating potential for an improved dosing regimen and side effect profile
• Plasma exposure observed to increase in accordance with dose. With a potential improved dosing regimen and side-effect profile in combination with the ability to treat patients with MGMT-resistant tumors, clinical trial data for VAL-083 is encouraging for this new chemotherapeutic in development to treat glioblastoma.
NEW THERAPIES TO TREAT GLIOBLASTOMA ARE URGENTLY NEEDED
As we have reviewed, glioblastoma is one of the most common and fatal brain cancers, and new therapies to treat this disease are urgently needed. New approaches, such as vaccines and immunotherapies, have promising results, and to be most effective, will need to be used in combination with a chemotherapeutic, such as VAL-083. Thus, VAL-083 provides a promising and effective strategy for new single and combination therapies for GBM and other cancers.
With about 15,000 patients with glioblastoma in the US alone, there is clearly an unmet need for more effective therapies. In particular, therapies are needed that can further extend the life span of patients diagnosed with this disease, significantly improve the overall quality of their extended survival time, and ultimately, in coordination with adjunctive therapies, aim to provide a cure.
REFERENCES
1. Wedro B, Stöppler MC. (2009, Aug 26) Senator Ted Kennedy: Seizure, Brain Cancer, & Death. Retrieved June 17, 2013, from http://www.medicinenet.com/script/main/art.asp?articlekey=89633.|
2. Clarke J, Butowski N, Chang S. Recent advances in therapy for glioblastoma. Arch Neurol. 2010;67(3):279-283.
3. Binello E, Germano IM. Targeting glioma stem cells: a novel framework for brain tumors. Cancer Sci. 2011;102(11)1958-1966.
4. Ohka F, Atsushi A, Wakabayashi T. Current Trends in Targeted Therapies for Glioblastoma Multiforme. Neurology Research International; 2012: Article ID 878425, 13 pages. Hindawi Publishing Corporation. doi:10.1155/2012/878425.
5. Clarke J, Iwamoto FM, Sul J, Panageas K, Lassman AB, DeAngelis LM, Hormigo A, Nolan CP, Gavrilovic I, Karimi S, Abrey LE. Randomized phase II trial of chemoradiotherapy followed by either dose-dense or metronomic temozolomide for newly diagnosed glioblastoma. J Clin Oncol. 2009;27(23):3861-3867.
6. Quinn JA, Jiang SX, Reardon DA, Desjardins A, Vredenburgh JJ, Rich JN, Gururangan S, Friedman AH, Bigner DD, Sampson JH, McLendon RE, Herndon II JE, Walker A, Friedman HS. Phase II trial of temozolomide plus O6-benzylguanine in adults with recurrent, temozolomide-resistant malignant glioma. J Clin Oncol. 2009;27(8):1262-1267.
7. McDonald A, Isaacson J. Data Released at ASCO Demonstrates the Severe Unmet Need in Brain Cancer; DelMar Presented Promising Early Data. LifeSci Advisors Equity Research. Retrieved June 17, 2013, from http://lifesciadvisors.com/clients/delmar.
8. Cedars-Sinai Medical Center (2012, August 15). Vaccine targets malignant brain cancer antigens, significantly lengthens survival. ScienceDaily. Retrieved June 17, 2013, from http://www.sciencedaily.com/releases/2012/08/120815093108.htm#.Ubz_MWPfNI0.email.
9. Phuphanich S, Wheeler CJ, Rudnick JD, Mazer M, Wang HQ, Nuño MA, Richardson JE, Fan X, Ji , Chu RM, Bender JG, Hawkins ES, Patil CG, Black KL, Yu JS. Phase I trial of a multi-epitope-pulsed dendritic cell vaccine for patients with newly diagnosed glioblastoma. Cancer Immunol Immunother. 2013;62:125- 135.
10. Choi BD, Sanchez-Perez LA, Sampson JH. (2011, Dec 21) Glioblastoma Vaccines and Immunotherapeutic Approaches. Medscape Education Oncology. Retrieved June 19, 2013, from http://www.medscape.org/viewarticle/755576.
11. Grady D. (2009, Nov 17) Breaching a Barrier to Fight Brain Cancer. The New York Times. Retrieved June 17, 2013, from http://www.nytimes.com/2009/11/17/health/17tumor.html. 12. Bruce J. (2009, Sep 25). Surgeon Develops New Treatmants for Glioblastoma. Retrieved June 18, 2013, from http://nyp.org/advances/new-treatmentsglioblastoma.html.
Jeffrey Bacha is a seasoned executive leader with nearly 20 years of life sciences experience in the areas of operations, strategy, and finance. He is currently president, CEO, and co-founder of DelMar Pharmacueticals and serves as a director of Sernova Corp. Prior to this, he was the founding CEO of Inimex Pharmaceuticals Inc. and co-founder of XBiotech and Urigen Holdings Inc. Mr. Bacha has been recognized as a Top 40 Under 40 executive by Business in Vancouver magazine and is active in the community through volunteerism with the Leukemia & Lymphoma Society’s Team in Training program and as chairman of the Board for Covenant House Vancouver, an organization dedicated to assisting at-risk and homeless youth to re-enter society. He earned his MBA from the Goizueta Business School at Emory University and his BSc in biophysics/pre-med from the University of California, San Diego.
Total Page Views: 2296