Issue:March 2023
DELIVERY TECHNOLOGY - NeuroDirect™ Ketamine: Novel, Non-Systemic Topical Therapy for PTSD & Associated Intractable Depression
INTRODUCTION
PTSD, Post-Traumatic Stress Disorder, is a brain memory processing disorder that continues to affect emotions, thought processes, and behaviors such that normal functioning becomes difficult, if not impossible, in affected individuals. Many, particularly war veterans, resort to suicide as a means to escape its overwhelming effects.1-5
Patients with PTSD have in common experiences with profound associated psychological stress that remains embedded in their memory and continues to playback in various ways, influencing their mental well-being and functioning. There may also be associated physical aspects to the event that contribute to the process, such a sexual assault, physical abuse, head injury, or other trauma. But most important are the emotionally traumatizing aspects of the event that remain unresolved in the affected person’s psyche.6-7
Symptoms of PTSD are varied, and pharmaceuticals are generally used to specifically treat them. Counseling and bio-feedback are also used as augments. Symptoms may include flashbacks and uncontrollable thoughts about the event, nightmares, and severe anxiety. PTSD symptoms are generally grouped into four types: intrusive memories, avoidance, negative thinking and mood, or changes in emotional reactions.1,4,8,9
Although medications benefit in reducing PTSD symptoms, no single effective drug treatment for PTSD exists. Positive symptoms, such as re-experiencing, hypervigilance, and increased arousal, respond better to medication than negative ones of avoidance and withdrawal. As residual symptoms in spite of medications are the rule, much research continues in PTSD symptom management.10-12
SSRIs (selective serotonin reuptake inhibitors) have been considered first-line drug treatment. Data exists to support use of the following SSRIs: citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline. Bupropion and the SNRI venlafaxine have the lowest patient drop-out rates due to medication side-effects.13-17
In addition to antidepressants and benzodiazepines, anticonvulsants and other non-traditional compounds have been used in treating PTSD symptoms. Commonly used anticonvulsants include Carbamazepine, Topiramate, Lamotrigine, and Valproic Acid, which help reduce mood swings, agitation, impulsivity, and aggression. Narcotics and opioids are used for physical pain related to physically traumatic events.18-40
From the above, it is apparent the majority of patients with intractable symptoms of PTSD are on several different medications or “poly-pharmacy.” Not only are symptoms not adequately relieved, but side effects and drug-drug interactions can be problematic. This has led many patients to self-medicate with alcohol, cannabis, and off-the-street narcotics and psychedelics. Psychedelics include LSD, psilocybin (“magic mushrooms”), cocaine, and ketamine (“Special K.”).41-45
KETAMINE
Ketamine was primarily developed for induction and maintenance of general anesthesia. It induces “dissociative anesthesia,” a trance-like state providing pain relief, sedation, and amnesia. It is distinguished from other general anesthetics in that respiratory functions are preserved. Cardiac status is unaffected with maintenance of normal blood pressure, making it ideal for traumatic situations with significant blood loss and circulatory compromise. It was extensively used for battlefield surgical anesthesia in the Vietnam War.
Ketamine was first synthesized in 1962 and approved in US in 1970. It has been regularly used on dogs and horses; therefore, called “horse tranquilizer.”46 Because of its safety profile, it is used in pediatrics.
At lower, sub-anesthetic doses, ketamine has shown promise for pain and treatment-resistant depression. However, its antidepressant effect after IV dosing diminishes with time and long-term repeated IV use has not been sufficiently studied. Ketamine infusion clinics have popped up at major cities in the US, indicating unmet needs in treating PTSD with traditional pharmaceuticals.
Infusions are expensive, ranging from $300-$2000 per IV infusion, depending on dose and indication for treatment. Each infusion lasts an hour or more followed by an observation period for vital signs and side effects. Psychiatric side effects are frequent as well as elevated blood pressure and nausea. Insurance does not cover the infusions, and therapy can be cost prohibitive.
Ketamine is reported to be a robust and rapid-acting antidepressant, although the effect is transient. IV ketamine in treatment-resistant depression usually results in improved mood within 4 hours, reaching peak at 24 hours. The effect is diminished at 7 days, and most patients relapse within 10 days, although for a significant minority, the improvement may last 30 days or longer. The challenge with IV ketamine treatment is what to do when its anti-depressive effect wears off. Maintenance IV therapy, from twice weekly to once every 2 weeks, appears promising but is a costly option.
Even at low sub-anesthetic intravenous doses, psychiatric side effects are prominent. A majority of patients report feeling “strange, spacey, woozy or floating” or having visual distortions or numbness. Also mentioned frequently is difficulty speaking, confusion, euphoria, drowsiness, and concentration problems. Psychotic symptoms such as “going into a hole, disappearing, feeling melting, experiencing colors, and hallucinations” are described by around 10% of people. Dizziness, blurred vision, dry mouth, hypertension, nausea, increased/decreased body temperature, or feeling flushed are common non-psychiatric side effects.
Adverse effects are most pronounced near end of infusion. They are significantly reduced by 1 hour and generally resolve by 4 hours. Accordingly, a several-hour period of observation is recommended after ketamine infusion. Patients are not recommended to drive home afterward.
Ketamine has not been approved as an antidepressant in the US, but the Canadian Network for Mood and Anxiety Treatments recommends it as a third line treatment for depression. An enantiomer of ketamine, esketamine, has been approved as a nasal spray for treatment-resistant depression in the US and elsewhere. Intravenous ketamine has not been directly compared with intranasal esketamine, but a comparative meta-analysis of clinical trials suggested IV ketamine’s superiority. There were greater overall response and remission rates and less dropouts from side effects.
Ketamine is used as a recreational drug in powder and liquid forms for its hallucinogenic and dissociative effects. At sub-anesthetic doses, ketamine produces a dissociative state, characterized by a sense of detachment from one’s physical body and the external world, known as “depersonalization” and “derealization.” At sufficiently high doses, users may experience what is called the “K-hole,” a state of dissociation with visual and auditory hallucinations similar to the effects of LSD.
Because of its ability to cause confusion and amnesia, ketamine has been used for date rape. Liver and urinary toxicities can occur with regular high-dose ketamine use, such as occurs in recreational use. Ketamine is an NMDA receptor antagonist, which may account for most of its actions. Its anti-depressive effects remain an area of debate and research. Ketamine is on the World Health Organization’s List of Essential Medicines and is available in generic form.47-50
NEURODIRECT™ KETAMINE AS NON-SYSTEMIC THERAPY
It is apparent ketamine can play an important role in treating intractable symptoms of PTSD. But, limiting use is expense, inconvenience of infusions, potential systemic side effects, and impracticality of maintenance therapy.
NeuroDirect™ (also known as Direct EffectsTM technology) is a novel, patented delivery of neuro-active compounds as cream applied to skin at the back of neck at the hairline (BONATH). BONATH is critical area of anatomy where access to afferent neural input to spinal cord and brain is achieved through Trigeminal and Vagal Nerve Complexes. Free nerve-endings under skin surface are activated by topically applied active drug, with neuro-chemical reactions occurring at specific receptors. Action potentials to central nervous system resulting from chemical reactions provide therapeutic benefit. This occurs without requirement of drug entry into bloodstream, a main source of side effects and drug interactions. The psychogenic effects encountered with intravenous and other systemic ketamine uses are avoided. With NeuroDirect technology, benefits of psychedelic compounds may be achieved without concern for their potential systemic effects.51
Neuro-active compounds that have been successfully used with NeuroDirect technology include: triptans, dopamine agonist apomorphine, tizanidine, phentermine, 4-amino pyridine; cannabinoids, in particular, CBD,CBG, and beta-caryophyllene; as well as opioids, amantadine, tramadol, and others. In all these topical drug applications, therapeutic benefit was generally noted within 10-15 minutes of application, as nerve impulses from skin-free nerve-endings to brain travel at essentially the same rate for all individuals. Such is not so when gastrointestinal absorption and blood flow factors are involved, which even differ in an individual, depending on gastrointestinal and hemodynamic functions at the time.
With bloodstream not involved, none of the usual systemic side effects associated with these compounds have been observed in patients using NeuroDirect technology. A blood level study with migraine drug, sumatriptan/Imitrex™, revealed no presence of active compound in blood in all studied patients, suggesting therapeutic mechanism was by direct nerve connections without involvement of bloodstream or blood-brain-barrier.52-54 With sumatriptan pill, injection, or nasal spray, a “therapeutic blood level” is required for efficacy.
UNIQUE NATURE OF NEURODIRECTTM TOPICAL KETAMINE THERAPY FOR PTSD
Antagonism of NMDA receptor is thought responsible for anesthetic, analgesic, and psychomimetic effects of ketamine. Analgesia occurs through prevention of central sensitization in spinal dorsal horn neurons interfering with pain transmission to the brain. Ketamine’s antidepressant mechanism of action is less certain. It is likely the NMDA receptor is not solely responsible and other receptors are involved. NMDA receptors exist on peripheral nerves and skin-free nerve-endings, allowing receptor antagonism to occur at these sites with topically applied drugs such as ketamine. This allows for ketamine’s benefits in pain, depression, and anxiety relief associated with PTSD.49-50
In summary, through mechanisms at NMDA receptors, various chemical and neuro-electrical processes responsible for symptoms related to PTSD may be addressed using a single compound, ketamine. Additionally, using ketamine with NeuroDirect drug delivery technology allows potential undesirable side effects to be avoided, with therapeutic benefits achieved rapidly.
NEURODIRECT™ KETAMINE OBSERVATIONAL CLINICAL DATA
Observational data from an out-patient Neurology and Neuropsychiatry practice in 100 patients with intractable depression, anxiety, and other symptoms commonly associated with PTSD, indicated relief of symptoms with NeuroDirect ketamine applied as a cream on skin at BONATH. Initial dose was 100 mg/ml; but subsequently, with a different formulation, 25 mg/ml was found equally effective. Initial and maintenance dose is now 25-50 mg/ml depending on patient need. Subjects were patients with symptoms related to PTSD for a long time, having failed numerous previous other treatments. Many were significantly symptomatic while on several pharmaceuticals as well as herbal products, such as CBD and cannabis.
Discernible improvement in anxiety, depression, paranoia and unrealistic fear, focusing issues, cloudy thinking, neuropathic pain, and other such symptoms were noted within 8-10 minutes of topical drug application. Benefit by patients was also noted by family members and other objective observers. In some instances, clinical improvement was documented by objective measures, such as the Hamilton Depression Scale and EEG tracings.
More than 80% of patients trying NeuroDirect topical ketamine found it effective to the extent formal prescriptions were requested for continued use at home. As with any therapeutic intervention, patient selection is key in determining clinical response. No psychogenic effects, such as hallucinations or dissociative phenomena, were experienced by any patient. To the contrary, patients indicated their thought processes were clearer, more focused; and, that they were more keenly aware of surroundings.
Initial ketamine dose was 25-50 mg: 1-2x/day. Less “wearing off” phenomena with return of symptoms was seen with longer continued use, suggesting “de-programming” of PTSD-related neural circuits. Some patients reduced dosing after 2-3 weeks. After a period, some patients were even able to change to use on “as needed basis.” In more severe chronically affected individuals, 25-50 mg every 2-3 days was generally required as maintenance therapy. Using the NeuroDirect topical ketamine, a significant number of patients were able to reduce or discontinue prior medications.
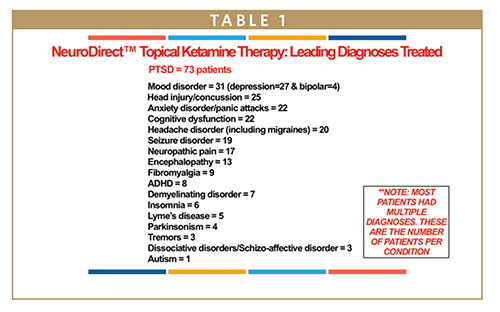
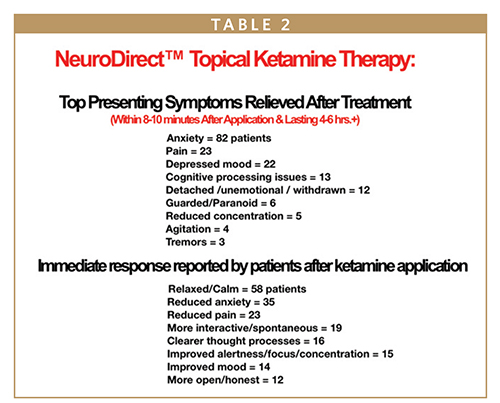
Table 1 provides a breakdown of diagnoses of the 100 treated patients. Middle- aged females with PTSD predominated; there were 61 females and 39 males. Ages ranged from 12 to 90 years. Table 2 shows top presenting symptoms relieved by ketamine therapy and immediate responses noted.
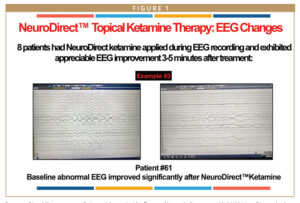
Eight patients had NeuroDirect ketamine applied during EEG recording. All exhibited EEG improvement 3-5 minutes after treatment. Figure 1 is an example one such patient.
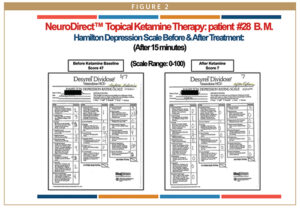
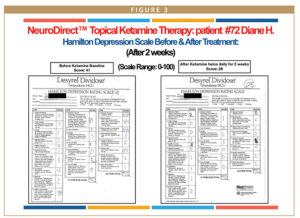
The Hamilton Depression Rating Scale (HAM-D) is a multiple-item questionnaire that provides indication of depression and guides in evaluating treatment response and recovery. The questionnaire is self-assessed, with occasional input of a significant other/spouse/family member as corroboration. It rates severity of depression, anxiety, and other symptoms that may be associated with PTSD. It evaluates mood, feelings of guilt, suicide ideation, insomnia, agitation, retardation, anxiety, weight loss, and other somatic symptoms.
Figures 2 and 3 show changes in the Hamilton Depression Scale in two patient examples. One is immediately after ketamine application, and the other, 2 weeks after continuous twice-daily therapy. Six patients studied before and after treatment with ketamine, exhibited reduction in HAM-D scores of 40, 22, 13, 11, and 7 points 15 minutes after ketamine application.
SUMMARY
In view of the preliminary observational data, formal controlled studies need to be undertaken and steps taken to make this revolutionary product more widely available. It is more cost-effective, convenient, and appears more effective than currently available treatments using systemic ketamine for PTSD symptoms. Additionally, there is no concern for psychogenic and other systemic effects.
The following is a testimonial from a patient who used NeuroDirect ketamine: “It was like truth serum! I became aware of thoughts and emotions I had suppressed which needed to come out. I found myself crying uncontrollably as I released them. It allowed me to move forward as I had been stuck in a rut. I began to feel so much better as I faced how selfishly and un-lovingly I had treated my ill mother before she suddenly passed away.” Another stated “The usual triggers no longer affected me to go into a panic state…”
REFERENCES
- Post-traumatic stress disorder, Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Dec.13, 2016.
- Post-traumatic stress disorder. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd/index.shtml. Accessed Dec. 13, 2016.
- Posttraumatic stress disorder. National Alliance on Mental Illness. https://www.nami.org/Learn-More/Mental-Health-Conditions/Posttraumatic-Stress-Disorder/Support. Accessed Dec. 13, 2016.
- What is posttraumatic stress disorder? American Psychiatric Association. https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd. Accessed Dec. 13, 2016.
- Department of Veterans Affairs and Department of Defense. (2017). VA/DoD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. Author. Retrieved from: https://www.healthquality.va.gov/guidelines/MH/ptsd/.
- Coping with traumatic stress reactions. National Center for PTSD. http://www.ptsd.va.gov/public/treatment/cope/coping-traumatic-stress.asp. Accessed Dec. 13, 2016.
- Friedman, M. J. (2014). The human stress response. In N. C. Bernardy & M. J. Friedman (Eds.), A practical guide to PTSD treatment: Pharmacological and psychotherapeutic effects (pp. 9-20). American Psychological Association.
- Helping a family member who has PTSD. National Center for PTSD. http://www.ptsd.va.gov/public/family/helping-family-member.asp. Accessed Dec. 13, 2016.
- Rothbaum BO. Psychotherapy for posttraumatic stress disorder in adults. http//www.uptodate.com/home. Accessed Dec. 13, 2016.
- Clinician’s guide to medications for PTSD. National Center for PTSD. http://www.ptsd.va.gov/professional/treatment/overview/clinicians-guide-to-medications-for-ptsd.asp. Accessed Dec. 13, 2016.
- Lee, D. J., Schnitzlein, C. W., Wolf, J. P., Vythilingam, M., Rasmusson, A. M., & Hoge, C. W. (2016). Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: Systematic review and meta-analyses to determine first-line treatments. Depression and Anxiety, 33(9), 792-806. https://doi.org/10.1002/da.22511.
- Laddis, A. (2011). Medication for complex posttraumatic stress disorders. Journal of Aggression, Maltreatment & Trauma, 20(6), 645-668. https://doi.org/10.1080/10926771.2011.59613.
- Brady, K., Pearlstein, T., Asnis, G. M., Baker, D., Rothbaum, B., Sikes, C. R., & Farfel, G. M. (2000). Efficacy and safety of sertraline treatment of posttraumatic stress disorder: A randomized controlled trial. Journal of the American Medical Association, 283(14), 1837-1844. https://doi.org/10.1001/jama.283.14.1837.
- Marshall, R. D., Beebe, K. L., Oldham, M., & Zaninelli, R. (2001). Efficacy and safety of paroxetine treatment for chronic PTSD: A fixed-dose, placebo-controlled study. American Journal of Psychiatry, 158(12), 1982-1988. https://doi.org/10.1176/appi.ajp.158.12.1982.
- Davidson, J., Stein, D. J., Rothbaum, B. O., Pedersen, R., Szumski, A., & Baldwin, D. S. (2012). Resilience as a predictor of treatment response in patients with posttraumatic stress disorder treated with venlafaxine extended release or placebo. Journal of Psychopharmacology, 26(6), 778-783. https://doi.org/10.1177/02698811114138211.
- Martenyi, F., Brown, E. B., Zhang, H., Koke, S. C., & Prakash, A. (2002). Fluoxetine v. placebo in prevention of relapse in post-traumatic stress disorder. The British Journal of Psychiatry : The Journal of Mental Science, 181(4), 315-320. https://doi.org/10.1192/bjp.181.4.315.
- Friedman, M. J., Marmar, C. R., Baker, D. G., Sikes, C. R., & Farfel, G. M. (2007). Randomized, double blind comparison of sertraline and placebo for posttraumatic stress disorder in Department of Veterans Affairs setting. Journal of Clinical Psychiatry, 68(5), 711-720.
- Watts, B. V., Schnurr, P. P., Mayo, L., Young-Xu, Y., Weeks, W. B., & Friedman, M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 74(6), e541-550. https://doi.org/10.4088/JCP.12r08225.
- McElroy, S. L., Weisler, R. H., Chang, W., Olausson, B., Paulsson, B, Brecher, M., Agambaram, V., Merideth, C., Nordenhem, A., & Young, A. H. (2010). A double-blind, placebo-controlled study of quetiapine and paroxetine as monotherapy in adults with bipolar depression (EMBOLDEN II). Journal of Clinical Psychiatry, 71(2), 163-174. https://doi.org/10.4088/JCP.08m04942gre.
- Davidson, J., Baldwin, D., Stein, D. J., Kuper, E., Benattia, I., Ahmed, S., Pedersen, R., & Musgnung, J. (2006). Treatment of posttraumatic stress disorder with venlafaxine extended release: A 6-month randomized controlled trial. Archives of General Psychiatry, 63, 1158-1165. doi: 10.1001/archpsyc.63.10.1158.
- McRae, A. L., Brady, K. T., Mellman, T. A., Sonne, S. C., Killeen, T. K., Timmerman, M. A., & Bayles-Dazet, W. (2004). Comparison of nefazodone and sertraline for the treatment of posttraumatic stress disorder. Depression & Anxiety, 19(3), 190-196. https://doi.org/10.1002/da.20008.
- Davidson, J., Kudler, H., Smith, R., Mahorney, S. L., Lipper, S., Hammett, E., Saunders, W. B., & Cavenar, J. O. Jr. (1990). Treatment of posttraumatic stress disorder with amitriptyline and placebo. Archives of General Psychiatry, 47(3), 259-266. https://doi.org/10.1001/archpsyc.1990.01810150059010l.
- Petrakis, I. L., Ralevski, E., Desai, N., Trevisan, L., Gueorguieva, R., Rounsaville, B., & Krystal, J. H. (2012). Noradrenergic vs serotonergic antidepressant with or without naltrexone for Veterans with PTSD and comorbid alcohol dependence. Neuropsychopharmacology, 37(4), 996-1004. https://doi.org/10.1038/npp.2011.283.
- Frank, J. B., Kosten, T. R., Giller, E. L. Jr., & Dan, E. (1998). A randomized clinical trial of phenelzine and imipramine for posttraumatic stress disorder. American Journal of Psychiatry, 145(10), 1289-1291. https://doi.org/10.1176/ajp.145.10.1289.
- Becker, M. E., Hertzberg, M. A., Moore, S. D., Dennis, M. F., Bukenya, D. S., & Beckham, J. C. (2007). A placebo-controlled trial of bupropion SR in the treatment of chronic posttraumatic stress disorder. Journal of Clinical Psychopharmacology, 27(2), 193-197. https://doi.org/10.1097/JCP.0b013e318032eaed.
- Tucker, P., Trautman, R. P., Wyatt, D. B., Thompson, J., We,S. C., Capece, J. A., & Rosenthal, N. R. (2007). Efficacy and safety of topiramate monotherapy in civilian posttraumatic stress disorder: A randomized, double-blind, placebo-controlled study. Journal of Clinical Psychiatry, 68(2), 201-206. https://doi.org/10.4088/JCP.v68n0204.
- Andrus, M. R., & Gilbert, E. (2010). Treatment of civilian and combat-related posttraumatic stress disorder with topiramate. Annals of Pharmacotherapy, 44(11), 1810-1816.https://doi.org/10.1345/aph.1P163. 28. Davis, L. L., Davidson, J. R., Ward, L. C., Bartolucci, A., Bowden, C. L., & Petty, F. (2008). Divalproex in the treatment of posttraumatic stress disorder: a randomized, double-blind, placebo-controlled trial in a Veteran population. Journal of Clinical Psychopharmacology, 28(1), 84-88. https://doi.org/10.1097/JCP.0b013e318160f83b.
- Hamner, M. B., Faldowski, R. A., Robert, S., Ulmer, H. G., Horner, M. D., & Lorberbaum, J. P. (2009). A preliminary controlled trial of divalproex in posttraumatic stress disorder. Annals of Clinical Psychiatry, 21(2), 88-94. http://europepmc.org/article/MED/19439158.
- Davidson, J. R., Brady, K., Mellman, T. A., Stein, M. B., & Pollack, M. H. (2007). The efficacy and tolerability of tiagabine in adult patients with post-traumatic stress disorder. Journal of Clinical Psychopharmacology, 27(1), 85-88. https://doi.org/10.1097/JCP.0b013e31802e5115.
- Pae, C. U., Lim, H. K., Peindl, K., Ajwani, N., Serretti, A., Patkar, A. A., & Lee, C. (2008). The atypical antipsychotics olanzapine and risperidone in the treatment of posttraumatic stress disorder: A meta-analysis of randomized, double-blind, placebo-controlled clinical trials. International Clinical Psychopharmacology, 23(1), 1-8. https://doi.org/10.1097/YIC.0b013e32825ea324.
- Krystal, J. H., Rosenheck, R. A., Cramer, J.A., Vessicchio, J. C., Jones, K. M., Vertrees, J. E., Horney, R. A., Huang, G. D., & Stock, C. (2011). Adjunctive risperidone treatment for antidepressant-resistant symptoms of chronic military service-related PTSD. Journal of the American Medical Association, 306(5), 493-502. https://doi.org/10.1001/jama.2011.1080.
- Villarreal, G., Hamner, M. B., Cañive, J. M., Robert, S., Calais, L. A., Durklaski, V., Zhai, Y., & Qualls, C. (2016). Efficacy of quetiapine monotherapy in posttraumatic stress disorder: A randomized, placebo-controlled trial. American Journal of Psychiatry, 173(12),1205-1212. https://doi.org/10.1176/appi.ajp.2016.15070967.
- Raskind, M. A., Peskind, E. R., Hoff, D. J., Hart, K. L., Holmes, H. A., Warren, D., Shofer, J., O’Connell, J., Taylor, F., Gross, C., Rohde, K., & McFall, M. E. (2007). A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat Veterans with post-traumatic stress disorder. Biological Psychiatry, 61(8), 928-934. https://doi.org/10.1016/j.biopsych.2006.06.032.
- Simpson, T.L., Malte, C.A., Dietel, B., Tell, D., Pocock, I., Lyons, R., Varon, D., Raskind, M., & Saxon, A.J. (2015). A pilot trial of prazosin, an alpha-1 adrenergic antagonist, for comorbid alcohol dependence and posttraumatic stress disorder. Alcoholism: Clinical and Experimental Research, 39(5), 808-817. https://doi.org/10.1111/acer.12703.
- Amos, T., Stein, D. J., & Ipser, J. C. (2014). Pharmacological interventions for preventing post-traumatic stress disorder (PTSD). Cochrane Database of Systematic Reviews 2014, Issue 7, Art. No.:CD006239. https://doi.org/10.1002/14651858.CD006239.pub2.
- Braun, P., Greenberg, D., Dasberg, H., & Lerer, B. (1990). Core symptoms of posttraumatic stress disorder unimproved by alprazolam treatment. Journal of Clinical Psychiatry, 51(6), 236-238. https://search.proquest.com/docview/42392451?accountid=28179.
- Guina, J., Rossetter, S. R., DeRHODES, B. J., Nahhas, R. W., & Welton, R. S. (2015). Benzodiazepines for PTSD: A systematic review and meta-analysis. Journal of Psychiatric Practice, 21(4), 281-303. https://doi.org/10.1097/PRA.0000000000000091.
- Aerni, A., Traber, R., Hock, C., Roozendaal, B., Schelling, G., Papassotiropoulos, A., Nitsch, R. M., Schnyder, U., & de Quervain, D. J. (2004). Low-dose cortisol for symptoms of posttraumatic stress disorder. American Journal of Psychiatry, 161(8), 1488-90. https://doi.org/10.1176/appi.ajp.161.8.1488.
- McAllister, T. W., Zafonte, R., Jain, S., Flashman, L. A., George, M. S., Grant, G. A., He, F., Lohr, J. B., Andaluz, N., Summerall, L., Paulus, M. P., Raman, R., & Stein, M. B. (2015). Randomized placebo-controlled trial of methylphenidate or galantamine for persistent emotional and cognitive symptoms associated with PTSD and/or traumatic brain injury. Neuropsychopharmacology 41(5), 1191-1198. https://doi.org/10.1038/npp.2015.282.
- Neumeister, A. (2013). The endocannabinoid system provides an avenue for evidence-based treatment development for PTSD. Depression & Anxiety, 30, 93-96. https://doi.org/10.1002/da.22031.
- Bonn-Miller, M. O., Boden, M. T., Vujanovic, A. A., & Drescher, K. D. (2013). Prospective investigation of the impact of cannabis use disorders on posttraumatic stress disorder symptoms among Veterans in residential treatment. Psychological Trauma: Theory, Research, Practice, and Policy, 52(2), 193-200. https://doi,org/10.1037/a0026621.
- Neumeister, A., Normandin, M. D., Pietrzak, R. H., Piomelli, D., Zheng, M. Q., Gujarro-Anton, A., Potenza, M. N., Vailey, C. R., Lin, S. F., Najafzadeh, S., Ropchan, J., Henry, S., Corsi-Travali, S., Carson, R. E., & Huang, Y. (2013). Elevated brain cannabinoid CB1 receptor availability in post-traumatic stress disorder: A positron emission tomography study. Molecular Psychiatry, 18(9), 1034-1040. https://doi.org/10.1038/mp.2013.61.
- Psychedelics show promise in treating mental illness, Alternative & Complementary Therapies, MedicalXpress Breaking News-and-Events, November 19, 2021.
- Psychedelics, Nichols,D., Pharmacol Rev. 2016 April; 68(2): 356.
- Ketamine, Wikipedia.
- Feder, A., Parides, M. K., Murrough, J. W., Perez, A. M., Morgan, J. E., Saxena, S., Kirkwood, K., Aan Het Rot, M., Lapidus, K. A., Wan, L. B., Iosifescu, D., & Charney, D. S. (2014). Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: A randomized clinical trial. JAMA Psychiatry, 71(6), 681-688. https://doi.org/10.1001/jamapsychiatry.2014.62.
- Ketamine benefits neurocognition in depression with suicidal ideation, Keilp JG, et al. J Clin Psychiatry. 2021;doi:10.4088/JCP.21m13921.
- Ketamine Therapy for Bipolar Disorder, Jain, R., Psych Congress Network, 11/17/2021.
- What ketamine actually does to the brain, Yin, H., New Frontiers Psychiatric & TMS,2021.
- Aung-Din R. Topical regional neuroaffective (TRNA) therapy: novel groundbreaking triptan drug delivery for treating migraines. Drug Dev & Del. 2009;9(9):44-51.
- Aung-Din R, Davis T. Blood Studies Suggest Direct Neural Effect as Mechanism for Nuchal Topical Sumatriptan. Submitted Abstract. Headache Update 2014, Diamond Headache Clinic Annual Meeting, Orlando, FL, July 17-20, 2014.
- Aung-Din R. Nuchal topical neuro-affective therapy: a novel treatment for Parkinson’s disease using apomorphine. Drug Dev & Del. 2010;10(8):48. Issue: June 2016, Posted Date: 6/1/2016.
- Direct Effects™ Cannabinoid Therapy: Medical Cannabis Without Psychoactive & Systemic Effects, THERAPEUTIC FOCUS, Drug Dev & Del., June 2016.

Dr. Ronald Aung-Din practices General Neurology & Neuro-Psychiatry in Sarasota, FL. He is board-certified by the American Board of Psychiatry & Neurology and member, American Academy of Neurology. After earning his Bachelor’s and Master’s degrees in Engineering at Bucknell and Cornell Universities, he worked for a period as a supervising engineer. He then attended Columbia University in New York City for Premedical studies, followed by Medical School at University of Texas Southwestern Medical School, Dallas, TX. Residencies in Neurology and Neurosurgery were at University of Florida. Other studies included a Medical Student Fellowship in Cardiology at Radcliffe Infirmary, Oxford and Clinical Neurology Fellowship at National Hospital for Nervous Disease, Queen Square, London, UK. He has participated in over 60 pharmaceutical industry-sponsored clinical trials, functioning as Principal Investigator in drug research studies in MS, epilepsy, pain, Parkinson’s disease, and other neurological diseases. He is also active in treating varied neurological and psychiatric conditions using delivery of CNS-active drugs with Neuro-Direct™ technology, developed by him for which 13 US and foreign patents have been granted; with others pending. Publications using this novel therapy in migraine, Parkinson’s disease, autism spectrum disorder, and diabetic neuropathy; in addition to articles on the use of cannabidiol, CBD, and the non-cannabis cannabinoid receptor agonist, caryophyllene, have appeared in Drug Development and Delivery. AfGin Pharma, LLC was founded by Dr. Aung-Din in 2009 to advance his unique technology and its goal of “Enhanced Neuro-Therapeutics through Direct Effects Topical Technology.”

Dr. Chantelle G. Martin was born in Zimbabwe, Africa, and attended Medical School at the University of the Free State, Bloemfontein, South Africa, earning her Bachelor of Medicine and Bachelor of Surgery degree in 2016. She later completed 2 years of internship training at Grey’s Hospital, Pietermaritzburg, South Africa; rotating through Surgery, Pediatrics, OB-GYN, Neurology, Internal Medicine, Orthopedics, Anesthesiology, Family Medicine and Psychiatry, where she managed a wide range of medical and surgical conditions. Later, she also did a year of rural community service as a medical officer in Pietermaritzburg. She currently lives in Sarasota, FL, awaiting a residency position. In the interim she is not only gaining valuable clinical experience but also participating in groundbreaking research with the General Neurology and Neuropsychiatry clinical research practice of Sarasota neurologist Dr.Ronald Aung-Din and his AfGin Pharma, LLC research and development bio-pharmaceutical company, founded in 2009. Her recent work with the Direct Neuro Topical use of ketamine for the treatment of PTSD and intractable depression is an example of the value she provides in clinical research, advancing novel non-systemic technologies for difficult neurological and psychiatric disorders. Her passion for finding treatments for diseases of the nervous system using neuro-psychotropic drugs is evident and an added bonus to her contribution to medical pharmaco-therapeutics.
Total Page Views: 10737