Issue:May 2017
ASSAY VALIDATION - Biomarker Assay Validations – A Time for Change?
INTRODUCTION
Biomarkers have been used for many years in drug development and delivery for a wide range of clinical utilities, and throughout the past decade, their use has substantially increased. To accurately assess the measurement performance and characteristics and determine the range of conditions under which the biomarker will provide reproducible and accurate data, analytical methods for biomarkers must be validated. In 1991, the Food and Drug Administration (FDA) made new guidance available for bioanalytical method validation, which informed all laboratories doing bioanalysis how they should validate their scientific methods, its central focus being on methods for the evaluation of Pharmacokinetics (PK) – [Guidance updated 2001 & 2013 (draft)]. Since that time, it has been the “holy grail” for almost all researchers working in this scientific arena. However, it has also been used by many laboratories in the same way for validating biomarker assays for drug discovery and development. Recently, there has been considerable debate within the community over whether the guidance is applicable or best scientific practice to areas outside of PK evaluation. The following explores these debates and consider whether it is time to re-evaluate the requirements for biomarker assay validation.

WHAT IS A BIOMARKER?
The World Health Organization (WHO) defines a biomarker as, “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacological responses to a therapeutic intervention.”1 In practice, biomarkers include tools and technologies that ultimately help to build an understanding of the prediction, cause, diagnosis, and progression of disease and the outcome of treatment.2
Molecular biomarkers can take many forms and have become a pivotal tool in basic and clinical research as well as in clinical practice. In today’s research environment, the use of biomarkers for many different clinical utilities in clinical trials has become widely accepted, and they are fast becoming an essential part of clinical development.
THE DRUG DISCOVERY & DEVELOPMENT LANDSCAPE
Almost 10 years ago, the pharmaceutical industry was facing a remarkably high attrition rate for drugs in clinical development. Multiple studies were reporting that clinical success rates across the drug industry could potentially be even lower than estimated previously.3 Despite major advances in the basic science of drug discovery and development, which led to a substantial increase in the number of new drug targets, the development of novel effective therapies did not appear to be following the same upward trajectory. In 2006, it was estimated that only 8% of tested products entering Phase I trials gained regulatory approval, and many of these failures happened in late-stage clinical trials.4 Additionally, very few drugs were making it out of the clinical research pipeline, and in 2007, the US FDA approved only 17 new molecular entities and two biologic licenses; the lowest number since 1983.5
The significant reduction in clinical success rates across the drug industry appeared to be caused by a gap in the industry’s ability to predict a drug candidate’s early performance. To counteract the downturn in novel effective therapies, it was suggested that biomarkers, typically used to monitor therapeutic progress, disease progression, and the efficacy of interventions, could provide a solution. Biomarkers were considered attractive as they may predict drug efficacy more quickly than conventional clinical endpoints, and have the potential to substantially accelerate production development in certain disease areas. Furthermore, by identifying candidates that are likely to fail earlier in the process, biomarkers can lead to a reduction in drug development costs. As the mantra goes with drug development: if you fail early, you fail cheap.6
Biomarker assay requirements are designed before clinical trials commence, and a new drug would not be developed without simultaneously looking for biomarkers for efficacy, safety, and to measure the pharmacodynamics (PD) of the drug. Other utilities are also used (depending upon the mode of action of the drug for instance). The field of oncology is leading the way in the use of biomarkers in drug development, and their use as an alternative to clinical endpoints in drug development has meant that oncology has not experienced the same downturn in drug development that has been experienced by other therapeutic areas. However, many of the biomarker determinations in this arena are not performed using “wet” methods for quantitative assays in biological fluids.
THE BIOMARKER VALIDATION CHALLENGE
Validation is the process of assessing the biomarker analytical method and its measurement performance characteristics, as well as determining the range of conditions under which the biomarker will give reproducible and accurate data.7 The validation of biomarker analytical methods is a crucial step in the quest to deliver high-quality research data, and the criteria for validation are defined by the following:
-The nature of the question that the biomarker is designed to address
-The degree of certainty that is required for the desired answer
-The assumptions about the relationship between changes in the biomarker and clinical endpoints or other clinical utilities (eg, mechanistic, PD, etc)8
Although it is perfectly clear that method validation is a crucial step when using biomarkers, there is an absence of official guidelines for the validation of biomarker assays. Since the FDA 2013 Draft guidance was published, its content in relation to biomarker assays has been the subject of wide and contentious debate within the industry. This ultimately has culminated in inconsistent adaptations of related regulations in bioanalytical and clinical laboratories. It has been agreed for many years that there is a lack of standardization between laboratories. This was the original motivation behind the FDA releasing the FDA Guidance for Industry for Bioanalytical Method Validation [originally 1991, updated 2001 and 2013 (draft)], as mentioned. Essentially, these documents have driven forward improvements in the standardization of bioanalytical methods, and researchers continue to use the FDA (and other regulators) guidance(s) today.
This guidance provides assistance to sponsors of investigational new drug applications (INDs), new drug applications (NDAs), abbreviated drug applications (ANDAs), and supplements in developing bioanalytical method validation information used in human clinical pharmacology, bioavailability (BA), and bioequivalence (BE) studies requiring pharmacokinetic (PK) evaluation. This guidance also applies to bioanalytical methods used for non-human pharmacology/toxicology studies and preclinical studies.
However, although the guidance has undoubtedly proven beneficial, it only addresses critically the validation of assays to support PK assessments. Despite the document implying its limited scope (above) for purposes other than PK evaluation, many laboratories still continue to use the guidance verbatim, as it seems to have been interpreted that it is the only way that analytical methods should be validated. As the use of biomarkers for drug development accelerated and some researchers continued to use the FDA guidance, many clinical scientists were simultaneously questioning the extensive and confusing application of the terms “biomarker” and “validation,” and whether this guidance was appropriate for biomarker analytical methods used in drug discovery and development.
ADDRESSING THE CHALLENGES
Successful validation requires an understanding of exactly what an analytical method is doing and how it works. Once this is known, experiments can be designed to test the method and prove the performance of the assay. A further step that needs to be considered when utilizing biomarkers is the clinical validity of the results. Validation should demonstrate that a method is “reliable for the intended application.” In 2000-2001, a group of scientists working under the auspices of the American Association of Pharmaceutical Scientists (AAPS) recognized that by following the FDA guidance for industry for the validation of Biomarker methods, we were often not able to answer the clinical questions being asked, nor ensure the delivery of the clinical utility of the biomarker being studied.
These scientists brought together by a Bioanalytical Focus Group of the AAPS wanted to publish a document to bring consensus as to how biomarker assays should be validated to ensure results obtained were clinically relevant. The outcome was a whitepaper titled Fit-for-Purpose Method Development and Validation for Successful Biomarker Measurement.9 This was the first seminal document that had been published on this subject (specifically for drug development) that highlighted a number of issues that have also been recognized in other white papers published since then: the “potential need to step out of the framework of regulated bioanalysis guidelines” as it was important to: “keep in mind the intended use of the data and the attendant regulatory requirements associated with that use.”
Ultimately, the whitepaper advised scientists how biomarker methods should be developed and validated when used in drug development as opposed to using them in diagnostics, to ensure that they were ‘fit-for-purpose.’ Many laboratories referred to this document and since Lee and colleagues published their whitepaper, the Global CRO Council (GCC) and European Bioanalysis Forum (EBF) also published papers on biomarker assay validation.10,11 Overall, there has been a drive forward in the number of laboratories demonstrating ways in which they generate improved data, thanks to this documentation being available (GCC survey 2016 – unpublished data).
TIME FOR A CHANGE
Despite an increase in awareness about biomarker assay validation, there are still multiple instances in which laboratories are obtaining incorrect, inaccurate, or variable results because they are following PK guidance documents for assay validation, which potentially can present a serious concern. The author has seen multiple examples in which biomarker results data has been generated that was incompatible with life, or inaccurate data has been produced that would lead to a false interpretation of the results from a clinical perspective. This is not good (nor acceptable) to the company developing the drug or the subjects participating in the clinical trials. This of course not only demonstrates the shortfalls of using a PK assay validation document for biomarker methods, but also that some bioanalytical laboratories do not have scientists with clinical knowledge that is crucial in the biomarker field. This is one of the reasons why understanding physiology and clinical biochemistry is so important to ensure that reliable and appropriate biomarker results data are generated using methods validated to appropriate standards.
By way of an example of one of the major issues from a clinical and scientific standpoint in using the PK guidance is that no weight is given to the different physiological changes seen in different biomarkers, nor the different performance characteristics of different methods when we set acceptance criteria for QC samples used when analyzing patient samples. The degree of change seen in different biomarkers is often specific to each biomarker from a clinical significance perspective – they are not all the same. For example, of ~400 biomarkers that are well characterized and understood, intra-individual variability in normal subjects range from <1% to >90%. Using PK guidance, however, the acceptance criteria for all the biomarkers using the same technology would be the same (eg, LC-MS/MS +/- 15% to 20%, and Immunoassay +/- 20% to 25%). Not only does this not make clinical sense, but it doesn’t add up statistically either because different analytical methods – even within the same technology – perform differently, and yet, the known analytical performance (from the validation experiments) is not being taken into account when setting acceptance criteria for QCs in sample batches. If acceptance criteria was primarily based on known method performance, this would prove methods are working as they should be but also give confidence limits around the results being reported, aiding statistical and clinical interpretation. In summary on this point, the concept of statistically valid Quality Control does not exist if we follow the guidance, and clinical relevance is not covered in any way in determining if the method is fit for its intended purpose.
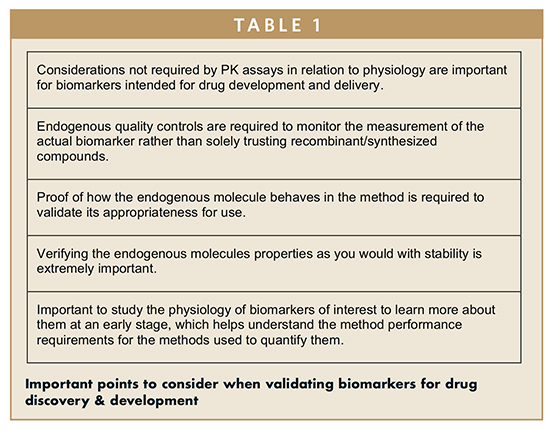
Discussions surrounding the topic of biomarker assays and validation continue to grow, and throughout the past 12 or more months, the industry has begun to speak out on the subject of biomarker assay validation in a unified way. In September 2015, the FDA and AAPS organized Crystal City VI, called in response to the previous meeting (Crystal City V).12 At Crystal City V, a revised version of FDA guidance published in 2013 was discussed. The document was a source of concern and disagreement from those involved in biomarker science, due to the content and also the recommendations within the paper with regard to biomarker assay validation guidance. At Crystal City VI, some very central points were raised.13 However, the major point that was raised by several key opinion leaders was that biomarker assays differ from PK assays, meaning that they should be validated in a different way. It was agreed that when using biomarkers for drug development and delivery, several important points should be considered (Table 1).
Crystal City VI appeared to be the first time there had been a major shift in momentum. It appeared that scientists were willing to speak out in a unified voice, and a large majority were giving the same message; it was time for a change to the current guidance. Crystal City VI was followed by a number of additional meetings (WRIB April 2016, AAPS-NBC May 2016, and EBF BM workshop June 2016), featuring discussions that expanded on the points raised, and questioned how we go about moving forward. Industry key opinion leaders (KOLs) are now at a point where they have identified and are in consensus that there are numerous issues that need to be addressed, and in order to do so, it would be beneficial for a different guidance document to be considered. The significant question within the industry now is how do we move forward?
The limited scope within the existing guidance for purposes other than PK evaluation and increasing use of biomarkers for drug discovery and development means we are now at a time at which, in my opinion, a change in industry guidance for biomarker assay validation is essential.
THE FUTURE OF BIOMARKER VALIDATION
Despite the increased use of biomarkers, it appears that many researchers are still continuing to use the FDA guidance document for validation even though it only critically addresses the validation of assays to support PK evaluation and also has a limited scope described within the document in terms of studies where it should be used.
There have been a number of clinical studies in which the data obtained has been unrepresentative and incorrect because the bioanalytical lab has followed PK guidance to validate their bioanalytical methods. This is extremely concerning and highlights the importance of ensuring that laboratories conducting research have a real investment in terms of the right team, who understand the clinical questions being asked, and have the know-how to develop and validate methods that will answer the necessary questions.
As researchers, our aim is to follow the principles of good science, and to ensure that the results obtained are clinically robust and relevant. The use of biomarkers for drug discovery and development is a hot topic within the industry, and the FDA guidance has been questioned on many occasions in relation to its use for the validation of Biomarker assays. Now is the time to listen to the questions that have been raised and work toward an updated recommendation from industry KOLs who hopefully regulators will consider in developing revised guidance documents that will improve the reliability of biomarker results and ultimately benefit overall advances in healthcare in assisting the development of new drugs.
REFERENCES
1. WHO International Programme on Chemical Safety Biomarkers in Risk Assessment: Validity and Validation. 2001. http://www.inchem.org/documents/ehc/ehc/ehc222.htm.
2. Mayeux R. Biomarkers: potential uses and limitations. NeuroRx. 2004;1(2):182-188.
3. Hay M, Thomas DW, Craighead JL, et al. Clinical development success rates for investigational drugs. Nature Biotechnol. 2014;32:40-51.
4. O’Connell D, Roblin D. Translational research in the pharmaceutical industry: from bench to bedside. Drug Discovery Today. 2006;11(17-18):833-838.
5. Hughes B. 2007 FDA drug approvals: a year of flux. Nature Reviews Drug Discovery. 2008;7:107.
6. Thomson Reuters. Biomarkers: An indispensable addition to the drug development toolkit. http://thomsonreuters.com/content/dam/openweb/documents/pdf/pharma-life-sciences/white-paper/biomarkersan-indispensable-addition-to-the-drug-development-toolkit.pdf.
7. Hunter DJ, Losina E, Guermazi A, Burstein D, et al. A pathway approach to biomarker validation and qualification for osteoarthritis clinical trials. Current Drug Targets. 2010;11(5): 536-545.
8. Rolan P. The contribution of clinical pharmacology surrogates and models to drug development – a critical appraisal. Brit J Clin Pharmacol. 1997;44(3):219-225.
9. Lee JW, Devanarayan V, Barrett YC, et al. Fit-for-purpose method development and validation for successful biomarker measurement. Pharmaceut Res. 2006;23(2):312-328.
10. Hougton R, Gouty D, Allinson J, et al. Recommendations on biomarker bioanalytical method validation by GCC. Bioanalysis. 2012;4(20):2439-2446.
11. Timmerman P, Herling C, Stoellner D, et al. European Bioanalysis Forum recommendation on method establishment and bioanalysis of biomarkers in support of drug development. Bioanalysis. 2012;4(15):1883-1894.
12. Smeraglia J, McDougall S, Elsby K, et al. AAPS and US FDA Crystal City V meeting on Quantitative Bioanalytical Method Validation and Implementation: feedback from the EBF. Bioanalysis. 2014;6(6):729-732.
13. Lowes S, Ackermann BL. AAPS and US FDA Crystal City VI workshop on bioanalytical method validation for biomarkers. Bioanalysis. 2016;8(3):163-167.
To view this issue and all back issues online, please visit www.drug-dev.com.

John L. Allinson is the Head of Biomarker Strategy of LGC and brings over 40 years of experience in developing and working with biomarkers, including their use in drug development across all therapeutic categories and phases of development. Before joining LGC, Mr. Allinson spent 22 years in NHS Clinical Pathology services before moving into the CRO industry, where he managed Central, Bioanalytical, and Biomarker Laboratories at a number of CROs. He was part of the AAPS Ligand Binding Assay Bioanalytical Focus Group (LBABFG) Biomarker Committee, which published the first consensus white paper on biomarker assay validation requirements in Drug Development, and was also co-author of the recently published first white paper on the Validation of Multiplexed Biomarker assays. He has been an invited presenter at over 50 international conferences and continues to present an educational workshop on Biomarker Assay Method Development and Validation at the World Biomarker Congress.
Total Page Views: 8343